If your child swallows the wrong medication, time is the most critical factor. Not minutes. Not seconds. Time between ingestion and professional help determines whether this becomes a scare or a tragedy. Every second counts, and panic will cost you those seconds. You don’t need to be a doctor. You need to know what to do next - and do it fast.
Step 1: Call Poison Control Immediately
Don’t wait. Don’t Google. Don’t call your pediatrician first. Pick up the phone and dial 13 11 26 - Australia’s Poison Information Centre. This number is free, available 24/7, and staffed by toxicology nurses who’ve handled thousands of cases just like yours. They don’t just give advice - they guide you through real-time decisions based on what your child swallowed, how much, and their age and weight.
While you’re on the phone, have the medication container in hand. Read the label out loud. Note the active ingredient (like acetaminophen or ibuprofen), the strength (e.g., 500 mg), and how many pills or milliliters are missing. If it’s a liquid, estimate how much was spilled or left in the bottle. This information saves precious minutes.
Don’t assume it’s harmless just because it’s "over-the-counter." A single adult-strength acetaminophen tablet can cause liver failure in a toddler. A child’s body processes drugs differently - and dangerously.
Step 2: Remove Any Remaining Substance - But Don’t Induce Vomiting
While you’re on the call with Poison Control, gently open your child’s mouth. Use your fingers to remove any visible pills, patches, or liquid. Don’t force it. Don’t stick your fingers deep. Just clear what’s loose. If a medicated patch is stuck to their skin, peel it off carefully - they’re often hidden in the mouth, behind the tongue, or on the roof of the mouth after being sucked on.
Here’s what you must NOT do: Never make your child vomit. Not with syrup of ipecac. Not with your finger. Not with salt water. Not with anything. Since 2004, every major medical organization - including the American Academy of Pediatrics and the Australian Poisons Information Centre - has banned home vomiting induction. Why? It doesn’t remove enough of the drug. It can cause choking. It can burn the throat or lungs if the substance is caustic. And it delays the real help: expert guidance.
Step 3: Watch for These Warning Signs - and Act Fast
Some children seem fine right after swallowing a pill. That’s dangerous. Many drugs act silently. Watch closely for these red flags:
- Difficulty breathing, gasping, or lips turning blue
- Unconsciousness or extreme drowsiness - not just sleepy, but hard to wake up
- Seizures or unusual twitching
- Pupils that are unusually large or tiny
- Excessive drooling, vomiting, or nausea lasting more than 20 minutes
- Cold, clammy skin or pale appearance
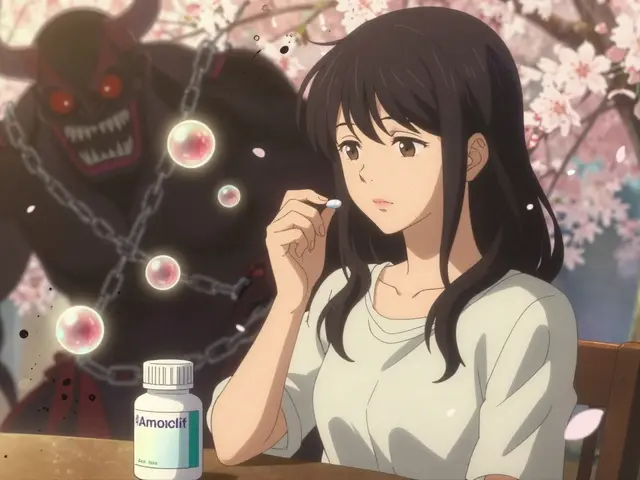
If any of these happen, call 000 immediately. Don’t wait for Poison Control to tell you to. This is a medical emergency. Cardiac medications like amlodipine can drop blood pressure below 70/40 mmHg in under 30 minutes. Acetaminophen overdose can silently destroy the liver. Your child doesn’t need to be screaming to be in danger.
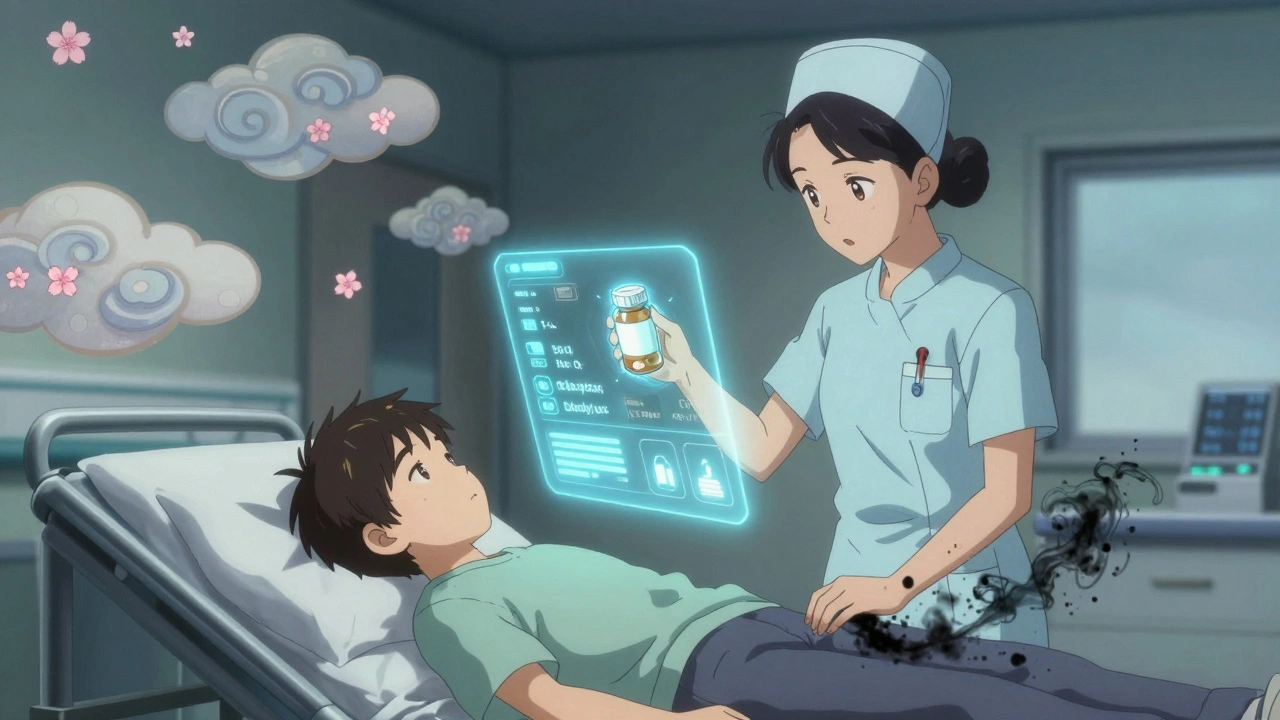
Step 4: What Happens at the Hospital?
Even if your child seems okay, most hospitals will keep them under observation for at least 12 hours after an unknown ingestion. Why? Some drugs take hours to show effects. Blood tests will check liver function, kidney levels, and glucose - especially if a diabetes medication was involved. Hypoglycemia from sulfonylureas can come on suddenly and cause seizures.
They may give activated charcoal - a fine black powder that binds to toxins in the stomach - but only if it’s been less than an hour since ingestion. For opioid overdoses, they’ll use naloxone - a fast-acting antidote that reverses breathing problems. For certain antidepressants or heart medications, they’ll monitor heart rhythm continuously and give IV fluids or sodium bicarbonate to stabilize electrolytes.
Don’t expect them to just "watch and wait." Modern poison management is precise. They’ll use the exact drug name, dose, and time of ingestion to calculate risk and choose treatment. That’s why having the container matters so much.
Why Most Parents Get It Wrong
A 2022 study found that 61% of Australian parents couldn’t recall the Poison Control number - even though they knew it existed. Meanwhile, 78% still believed outdated advice like using ipecac or making kids vomit. These myths come from old parenting books, well-meaning relatives, or social media posts that never got updated.
One mother on Reddit delayed calling for 45 minutes because she thought her 2-year-old was "just sleepy." The child had swallowed a single 10 mg amlodipine tablet. By the time they got to the hospital, the child’s heart rate had dropped to 42 beats per minute. They spent 36 hours in intensive care.
Another dad called Poison Control within 3 minutes after his child swallowed 3 antihistamine tablets. The nurse told him to keep the child awake, give sips of water, and monitor breathing. They didn’t go to the hospital. The child was fine by morning.
The difference? Action. Not waiting. Not guessing.
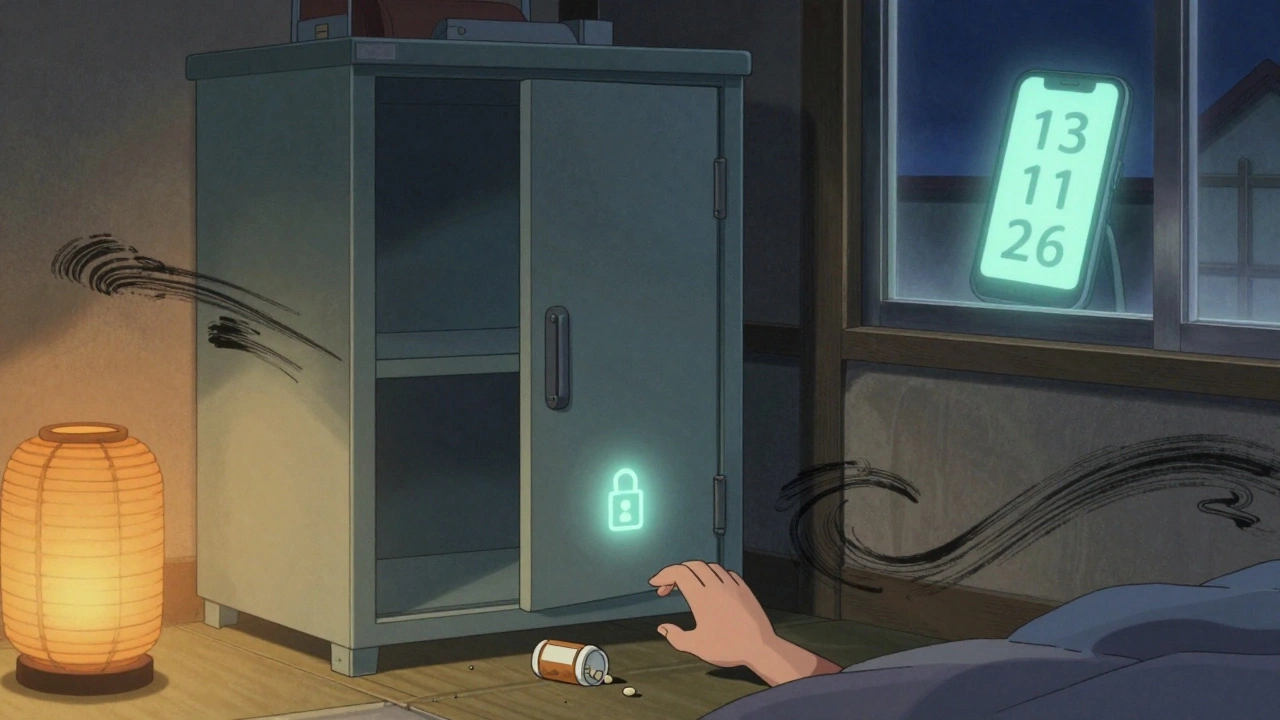
Prevention: How to Stop This From Happening Again
Once the crisis is over, the real work begins: preventing the next one.
- Store all medications - even vitamins and supplements - in locked cabinets, not on countertops or in bathroom drawers.
- Use child-resistant caps - but remember, they’re not child-proof. Toddlers can open them with enough time and persistence.
- Never take medication in front of children. If they see you swallow a pill, they’ll think it’s candy.
- Use a medication organizer with alarms, like Hero Health’s smart bottle, which locks and alerts you if someone tries to open it. It’s expensive - about $90/month - but cuts accidental access by 73% in studies.
- Check your home like a stranger would. Get down on your knees. Look at eye level. What’s within reach? A bottle of ibuprofen on the nightstand? A patch behind the toilet? Remove it.
The CDC found that homes with locked storage have 85% fewer accidental ingestions. That’s not a suggestion. That’s a lifesaver.
What’s Changing for the Future
In 2023, Australia adopted new child-resistant packaging rules requiring two independent safety mechanisms - like a push-and-turn cap plus a squeeze-and-lift seal. By 2025, this is expected to reduce accidental ingestions by 30%.
Online tools like webPOISONCONTROL now let parents input details about the substance and get instant, AI-powered guidance. It’s 94% accurate compared to human poison specialists. Use it - but never replace calling 13 11 26. The phone call gives you someone who can hear your child breathing, ask follow-up questions, and adjust advice in real time.
Research is also moving toward child-specific naloxone nasal sprays - already tested and approved for kids under 50 lbs. These could become standard in homes with opioid prescriptions.
But none of this matters if you don’t know what to do right now.
What should I do if my child swallows a pill but seems fine?
Call Poison Control at 13 11 26 immediately. Many dangerous drugs show no symptoms for hours. Even if your child is acting normal, they could be developing liver damage, low blood sugar, or heart problems. Don’t wait for signs. Get expert advice now.
Can I use ipecac to make my child vomit?
No. Ipecac has not been recommended for home use since 2004. It doesn’t remove enough of the poison, and it can cause serious harm - including aspiration pneumonia, choking, or worsening chemical burns. Poison Control will tell you exactly what to do - and it won’t involve vomiting.
What if I don’t know what my child swallowed?
Call Poison Control anyway. Bring all medication containers with you to the hospital. Even empty bottles, wrappers, or pill fragments help. The poison specialist will ask you questions about symptoms, timing, and possible substances to narrow down the risk. Don’t assume it’s nothing - act anyway.
Is it safe to wait and see if my child gets sick?
No. Some medications cause delayed effects. Acetaminophen can damage the liver in 24-48 hours. Heart medications can cause sudden cardiac arrest. Waiting is the most common mistake. Poison Control can tell you whether observation at home is safe - but only if you call right away.
How can I prevent this from happening again?
Store all medications in locked cabinets, out of reach and sight. Use child-resistant caps, but don’t rely on them alone. Never leave pills on counters or in purses. Teach children that medicine is not candy. Consider a smart pill dispenser like Hero Health if you have multiple medications in the home. The CDC says locked storage reduces incidents by 85%.
Should I take my child to the ER even if Poison Control says it’s okay?
If Poison Control says you can monitor at home, follow their instructions exactly. But if your child develops any symptoms - drowsiness, vomiting, trouble breathing, or confusion - go to the ER immediately. Poison Control gives you a plan, but your instincts matter too. If something feels wrong, trust it and go.
Final Thought: You’re Not Alone
Accidental medication ingestion is one of the most common pediatric emergencies - and one of the most preventable. You’re not a bad parent for this happening. You’re a parent who needs clear, fast, accurate information. And now you have it. Memorize 13 11 26. Put it on your fridge. Save it in your phone. Practice saying it out loud. Because when seconds matter, you won’t have time to look it up.





so i accidentally left my ibuprofen on the nightstand and my 2yo grabbed it… turned out to be just one pill but i still panicked. called 13 11 26 and the nurse was so chill. told me to watch for sleepiness and gave me a checklist. we’re fine now. thanks for the post.
yo if you’re not using activated charcoal within 60 minutes post-ingestion you’re already behind the curve. pharmacokinetics don’t lie. the absorption half-life of acetaminophen in toddlers is ~1.8h, so if you’re waiting for symptoms, you’re playing russian roulette with hepatic glutathione depletion. also, why the hell are people still using ipecac? it’s been obsolete since the 90s. poison control is the only legit first responder here.
MY SON ATE A BOTTLE OF VITAMINS ONCE AND I THOUGHT HE WAS JUST A LITTLE SLEEPY. THEN HE STARTED SHAKING AND I SCREAMED SO LOUD MY NEIGHBORS CALLED 911. TURNED OUT IT WAS JUST IRON OVERDOSE BUT THEY HAD TO GIVE HIM CHELATION THERAPY. I STILL HAVE NIGHTMARES. DON’T WAIT. DON’T GUESS. JUST CALL. 13 11 26 IS YOUR LIFELINE. 🙏
THIS IS SO IMPORTANT!!! 💪🔥 I JUST PUT LOCKED CABINETS IN EVERY ROOM NOW. EVEN THE BATHROOM. MY KIDS ARE 3 AND 5 AND THEY’RE LITTLE NINJAS. ALSO GOT A HERO HEALTH DISPENSER - IT’S WORTH EVERY DOLLAR. 🤖💊 #parentingwin
people still believe in ipecac? bro. it’s 2025. you’re not in a 1980s sitcom. if your kid swallows something, you don’t stick your finger down their throat - you call poison control and then drive. period. no drama. no myths. just action. this post saved lives. seriously.
oh wow. another ‘parenting guru’ telling everyone how to live. next you’ll tell us to stop breathing because oxygen is toxic in excess. 61% of parents don’t know the number? maybe because it’s a dumb number that doesn’t exist in the US. 13 11 26? that’s australian. are we supposed to fly to oz every time our kid sneezes near a pill?
the irony here is that the author cites australian guidelines while addressing an american audience. the poison control number referenced is not functional in the US. the correct number is 1-800-222-1222. this is not a minor error - it’s a critical misdirection. if someone follows this advice blindly, they could waste precious minutes dialing the wrong number. professionalism matters.
thanks for this. i’m a nurse and i’ve seen too many cases where parents waited because they thought it was ‘just a pill.’ i’ve been telling my friends to save the poison control number since my first kid was born. seriously, it’s on my phone’s lock screen. i’m so glad someone’s spreading this info.
you’re not alone. i used to think my child-resistant caps were enough. then my 18-month-old opened one in 47 seconds. i now use the hero health dispenser + locked cabinet + daily inventory check. it’s a system. prevention isn’t optional - it’s a daily practice. you’ve got this. keep learning, keep acting.
they’re hiding the truth. poison control is just a front for big pharma. the real danger is the chemicals they put in pills. why don’t you ask why they don’t make natural alternatives? why is there no warning about glyphosate contamination in acetaminophen? i’ve seen the documents. they’re covering it up. 13 11 26? that’s just a distraction. the real solution is hemp oil and fasting. i’ve saved three kids this way. just saying.
While the sentiment expressed herein is undoubtedly well-intentioned, the structural presentation lacks the requisite scholarly rigour. The use of colloquialisms and emotive punctuation undermines the authority of the guidance. Furthermore, the reference to an Australian helpline in an ostensibly international context constitutes a significant methodological flaw. One would hope for a more universally applicable, evidence-based protocol.
Wow. Just wow. You wrote an entire guide and didn’t even mention the fact that activated charcoal is contraindicated in hydrocarbon ingestions? Or that naloxone has a shorter half-life than most opioids? You’re giving parents half-baked info wrapped in urgency. This isn’t parenting advice - it’s a liability. Someone’s kid is going to die because they trusted this.
you think this post helps? i know a mom who called poison control and they told her to wait. her kid died. the nurse said "it’s probably just a vitamin." so now i don’t trust anyone. not doctors, not websites, not even my own instincts. we’re all just guessing until it’s too late.
you’re all missing the point. the real problem is that parents don’t even know what’s in their own medicine cabinet. i once found a 10-year-old bottle of Xanax in my kid’s backpack. no one ever threw it out. this isn’t about calling a number - it’s about cleaning up the mess we’ve made. and honestly? you’re all just waiting for the next tragedy to happen so you can feel guilty on Reddit.