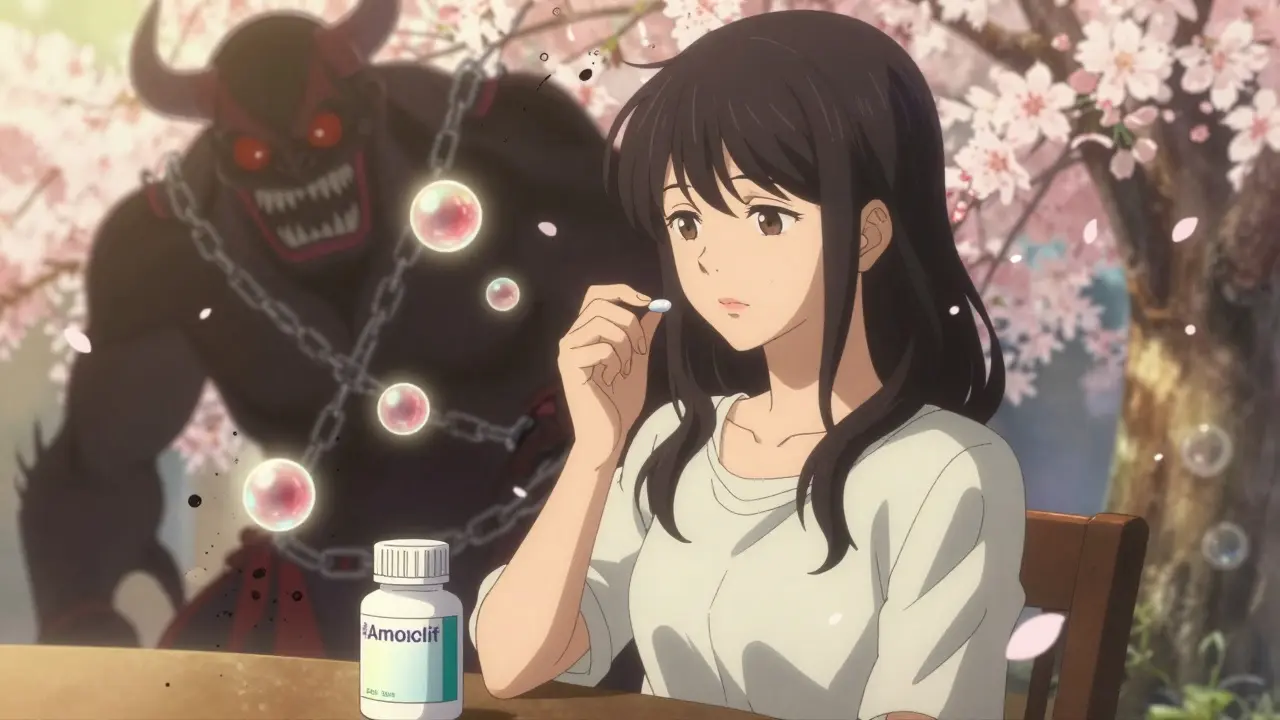
For decades, women have been told: antibiotics can mess with your birth control. You take amoxicillin for a sinus infection, and suddenly your pharmacist hands you a free pack of condoms with a serious look. But here’s the truth: for almost every antibiotic you’ll ever get, that warning is outdated, unnecessary, and based on a myth that won’t die.
Most Antibiotics Don’t Touch Your Birth Control
If you’re on the pill, patch, or ring, and your doctor prescribes amoxicillin, azithromycin, doxycycline, or ciprofloxacin, you don’t need to panic. None of these common antibiotics reduce the effectiveness of hormonal birth control. Decades of research confirm it. The CDC, ACOG, and major medical journals have all reviewed the data-and they agree: these drugs don’t interfere.
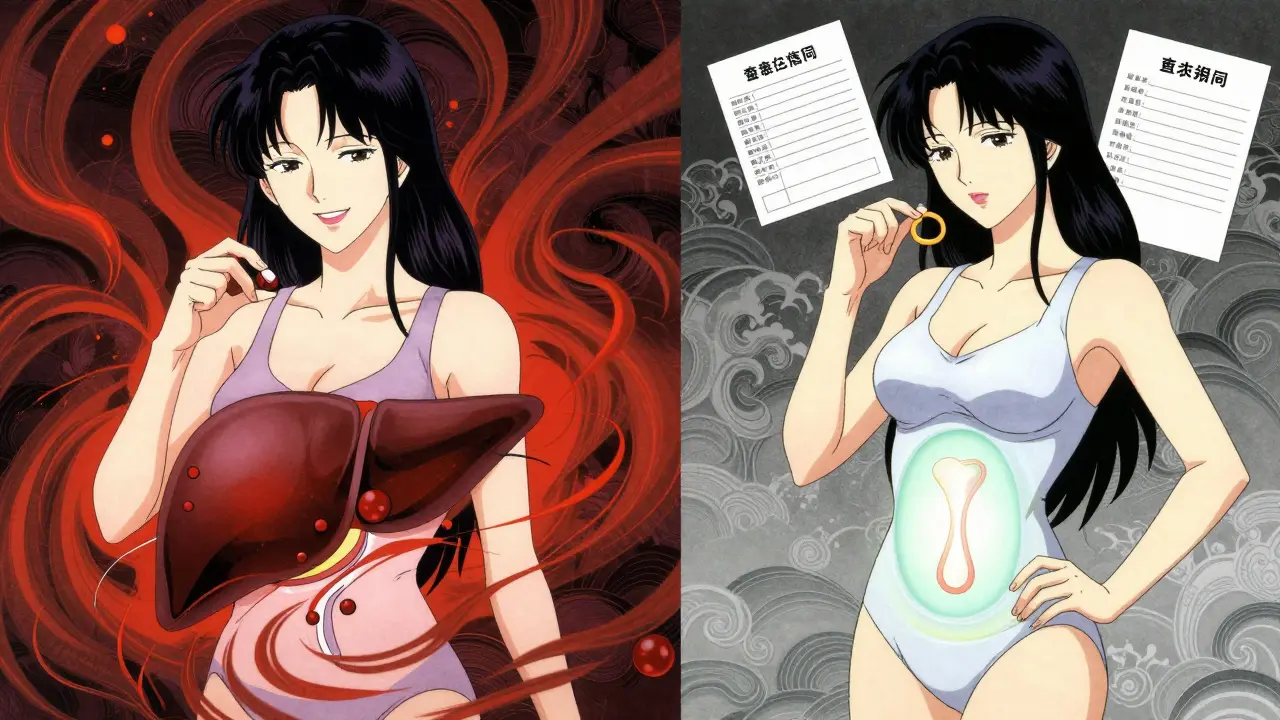
Here’s how it works: birth control pills rely on steady levels of hormones like ethinyl estradiol and progestin. These hormones are broken down in your liver. Some drugs speed up that process, lowering hormone levels enough to risk pregnancy. But most antibiotics? They just don’t do that. Studies tracking hormone levels in women taking amoxicillin or metronidazole showed no drop in contraceptive hormones. Serum estradiol stayed in the normal range-200 to 400 pg/mL-throughout treatment.
Real-world data backs this up. A 2011 review of 14 studies found no link between penicillin-type antibiotics and birth control failure. A 2020 CDC analysis of 35 clinical trials confirmed the same: non-rifamycin antibiotics never dropped hormone levels below the safe threshold of 50 pg/mL. And yet, 62% of women still believe antibiotics reduce effectiveness. That’s not because the science is unclear-it’s because the myth keeps getting repeated.
The One Antibiotic That Actually Does
There’s one big exception: rifampin. And its cousin, rifabutin. These are not your everyday antibiotics. They’re powerful drugs used to treat tuberculosis and some rare infections. Rifampin was first approved in 1967. Since then, we’ve known it changes how your body processes hormones.
Here’s the science: rifampin turns on liver enzymes-specifically cytochrome P450-by up to 300%. That means your body breaks down estrogen and progestin way faster. Studies show it can slash ethinyl estradiol levels by 25-50% and progestin by 14-37%. That’s enough to make birth control fail. There are documented cases of women getting pregnant while on rifampin, even while taking their pill correctly.
That’s why the CDC classifies rifampin and rifabutin as a Category 3 interaction-meaning the risk outweighs the benefit. If you’re prescribed one of these, you need backup contraception for 28 days after finishing the course. That’s not a suggestion. It’s a medical requirement.
Griseofulvin Is Also a Problem (Even Though It’s Not an Antibiotic)
Here’s a curveball: griseofulvin. It’s not an antibiotic. It’s an antifungal, used for stubborn fungal infections like ringworm or nail fungus. But it acts like rifampin-it boosts liver enzymes. So even though it’s not an antibiotic, it still reduces hormone levels enough to risk pregnancy.
WebMD and the CDC both say: if you’re on griseofulvin, use condoms or another backup method for a full month after your last dose. Don’t assume it’s safe just because it’s not called an antibiotic. The mechanism is the same.
What About Other Medications? You Might Be Surprised
Antibiotics aren’t the only drugs that can interfere. Some seizure meds do. Lamotrigine at doses over 300 mg/day and topiramate above 200 mg/day can lower hormone levels. So can certain HIV drugs like efavirenz and nevirapine. And then there’s St. John’s wort-the herbal supplement many take for mild depression. A 2017 study found it can drop estrogen levels by up to 57%.
That’s why it’s not just about antibiotics. It’s about enzyme inducers. Any drug that forces your liver to speed up hormone breakdown is a risk. Most antibiotics? Not on that list. But these other things? They are. If you’re on birth control and start any new medication-even something you bought over the counter-ask: “Does this make my liver work faster?”
Why Does This Myth Still Exist?
Back in the 1970s, a few case reports linked birth control failure with antibiotics. Those reports were messy. They didn’t control for vomiting, missed pills, or drug interactions. But the story stuck. Pharmacies kept handing out condoms. Doctors kept saying “just to be safe.”
Now, decades later, the evidence is clear. Yet, a 2022 Planned Parenthood survey found 62% of women still believe antibiotics reduce effectiveness. And 35% of pharmacists still recommend backup contraception for every antibiotic-even amoxicillin. Why? Because it’s easier to say “use a condom” than to explain enzyme induction.
Dr. Jen Gunter, an OB/GYN and author, calls it a “medical urban legend.” She says the myth persists because people remember the scary stories: “I got pregnant while on antibiotics.” But they forget the thousands of women who took amoxicillin ten times and never had an issue.
What Should You Actually Do?
Here’s the practical guide:
- If your antibiotic is amoxicillin, azithromycin, doxycycline, ciprofloxacin, metronidazole, clarithromycin, or erythromycin → No backup needed. Take your pill as usual.
- If your antibiotic is rifampin or rifabutin → Use condoms or another barrier method for 28 days after finishing the course.
- If you’re taking griseofulvin (for fungal infections) → Use backup for one month after treatment.
- If you’re taking lamotrigine, topiramate, efavirenz, nevirapine, or St. John’s wort → Talk to your doctor. You may need a different birth control method.
And if you’re unsure? Ask your pharmacist or doctor to name the drug’s exact class. If it’s a rifamycin or griseofulvin, ask about backup. If it’s anything else, you’re fine.

Confusion Between Rifampin and Rifaximin
One common mix-up: rifampin vs. rifaximin. They sound almost the same. But rifaximin (brand name Xifaxan) is used for traveler’s diarrhea and IBS. It doesn’t get absorbed into your bloodstream. It works only in your gut. So it doesn’t touch your liver enzymes. It doesn’t affect birth control. The FDA confirmed this in 2022. If your doctor prescribes rifaximin, you don’t need to change anything.
But if you hear “rif-” and panic, double-check the spelling. One letter changes everything.
What About Vomiting or Diarrhea?
Here’s another real risk: if you get sick. If you vomit within two hours of taking your pill, or have severe diarrhea, your body might not absorb the hormones. That’s not the antibiotic’s fault. That’s your gut. The CDC says: if you vomit or have diarrhea during antibiotic treatment, treat it like you missed a pill. Take another one as soon as you can, and use backup for the next seven days.
That’s why some providers still suggest backup during antibiotic use-not because of the drug, but because illness can disrupt absorption. It’s not about the antibiotic. It’s about your body’s reaction to infection.
Bottom Line: Know the Difference
Antibiotics are not all the same. Most are safe with birth control. Only rifampin, rifabutin, and griseofulvin are proven risks. The rest? They’re just treating your infection. Your birth control is still working.
Stop letting old myths dictate your choices. If you’re prescribed an antibiotic, ask: Is this rifampin? Is this griseofulvin? If not, you’re good. If yes, use backup. Simple. Clear. Evidence-based.
And if your pharmacist still hands you condoms for amoxicillin? Politely thank them, then ask if they’ve read the CDC’s 2021 guidelines. You might just help them update their practice too.
Do all antibiotics reduce the effectiveness of birth control pills?
No, only two types of drugs are proven to interfere: rifampin and rifabutin (used for tuberculosis), and griseofulvin (an antifungal). Common antibiotics like amoxicillin, azithromycin, doxycycline, and ciprofloxacin have been studied extensively and do not affect birth control hormone levels.
What should I do if I’m prescribed rifampin while on birth control?
Use a backup method of contraception-like condoms or a diaphragm-for 28 days after finishing your last dose of rifampin. This applies to all forms of combined hormonal birth control, including pills, patches, and vaginal rings. The CDC and ACOG both recommend this to prevent unintended pregnancy.
Can I rely on birth control if I have diarrhea or vomit while taking antibiotics?
If you vomit within two hours of taking your pill or have severe diarrhea, your body may not absorb the hormones properly. In that case, treat it like a missed pill: take another pill as soon as possible and use backup contraception for the next seven days. This risk comes from illness, not the antibiotic itself.
Is St. John’s wort safe to take with birth control?
No. St. John’s wort, a popular herbal supplement for mood, increases liver enzyme activity and can reduce estrogen levels by up to 57%. This can make birth control less effective. If you’re using hormonal contraception, avoid St. John’s wort unless your doctor advises otherwise.
Why do pharmacists still give out condoms with antibiotics?
Many pharmacists follow outdated guidelines or err on the side of caution because they’re afraid of liability. A 2022 study found 35% of pharmacists still recommend backup contraception for all antibiotics, even though medical guidelines say only rifampin and griseofulvin require it. The myth persists because it’s easier to give a condom than to explain enzyme induction.
Does the type of birth control matter? (Pill vs. IUD vs. shot)
Only combined hormonal methods-pills, patches, and vaginal rings-are affected by enzyme-inducing drugs like rifampin. Progestin-only pills, IUDs (hormonal or copper), implants, and shots are not impacted by these drugs. If you’re worried about interactions, switching to a non-hormonal or progestin-only method eliminates this risk entirely.





Finally, someone laid this out clearly. No more panic-buying condoms every time I take amoxicillin for a sore throat.
62% of women still believe this myth? That’s not ignorance-it’s systemic negligence. Doctors and pharmacists have been lazily perpetuating this for decades. If you’re not updating your practice based on CDC guidelines, you’re not a professional-you’re a liability.
Let’s be real-the whole ‘antibiotics ruin birth control’ thing is a cultural echo chamber. It started with one flawed case study in the 70s, got amplified by pharmacy liability fears, and now it’s gospel. But here’s the deeper truth: we’re conditioned to fear our own bodies. We don’t trust the science, so we clutch at condoms like security blankets. The real issue isn’t rifampin-it’s the medical industry’s failure to communicate nuance without inducing panic.
And don’t get me started on St. John’s wort. People pop it like candy because it’s ‘natural,’ but they’ll freak out if their pill gets flagged as ‘unsafe.’ Double standard much?
Also, rifaximin vs. rifampin? That’s not a typo-it’s a trap. One letter, two worlds. If your doctor can’t spell it right, how can you trust them with your reproductive health?
This isn’t just about birth control. It’s about how medicine weaponizes confusion to avoid accountability. We need better education, not more free condoms.
Women have been gaslit by medicine for generations. ‘Just use a condom’ is the modern version of ‘it’s all in your head.’ We’re told to trust science until it’s inconvenient-then we’re handed a plastic packet like children who can’t handle the truth. The fact that pharmacists still hand out condoms with amoxicillin isn’t caution-it’s condescension. And it’s rooted in the same patriarchal thinking that dismissed women’s pain for centuries. We don’t need more warnings. We need respect for our capacity to understand complex biology.
Progestin-only IUDs and implants are the real solution here. No enzyme interference. No myths. Just reliable, silent, effective autonomy. Maybe it’s time we stop asking permission and start demanding better tools.
Love this breakdown. So many people don’t realize that vomiting or diarrhea is the real culprit-not the antibiotic. I had a bad case of food poisoning last year while on the pill, panicked, and called my doctor. Turned out, it was the stomach bug, not the amoxicillin. That’s the distinction we need to spread. Knowledge > fear.
Okay but what if this is all a big pharma scam? What if they don’t want us to know that antibiotics DO interfere because they profit off of emergency contraception and new prescriptions? I’ve seen people get pregnant on amoxicillin. I know someone. It happened. And now they’re saying it’s ‘not possible’? That’s what they said about vaping and lung damage too. They always deny it until it’s too late. And what about the gut microbiome? If antibiotics kill your good bacteria, doesn’t that mess with hormone absorption somehow? No one talks about that. And what about the long-term effects of estrogen suppression? Are we being lied to again? I’m not buying it. I’m using condoms anyway. Better safe than sorry. And yes, I know they say ‘not proven’ but I’ve seen the stories. The stories are real. The data? Maybe not.
Also, St. John’s wort is dangerous. I took it with my pill and got a blood clot. Coincidence? I don’t think so. The FDA doesn’t regulate herbs. They don’t care. They only care about profit. I’m not taking any risks. Ever again.
So many of us grew up with this fear whispered like a curse-antibiotics and pills don’t mix. But truth? It’s not magic. It’s biochemistry. And science? It’s kinder than our fears. I’m from India-where birth control is still taboo-and yet, here, in this post, I found freedom. No condoms. Just pills. Just trust. Thank you.
While the evidence presented is compelling, it is imperative to acknowledge that individual metabolic variations exist. Although population-level studies demonstrate no significant interaction between common antibiotics and hormonal contraceptives, pharmacokinetic differences due to genetic polymorphisms in CYP450 enzymes may result in atypical outcomes in isolated cases. Therefore, while generalized guidelines are clinically sound, personalized medical advice remains essential for risk mitigation in vulnerable populations.
Thank you for this. I’ve been telling my friends for years that amoxicillin doesn’t break the pill-but they still panic. I’m sharing this everywhere. Also, I switched to a copper IUD after learning about rifampin and St. John’s wort. Best decision ever. No stress. No myths. Just peace. 🌿