How Insurance Actually Covers Generic Drugs From Online Pharmacies
If you’re buying generic medications online and wondering whether your insurance will pay for it, you’re not alone. Many people assume that if a pharmacy is online, it automatically works with insurance. That’s not true. The difference between a mail-order pharmacy run by your insurance plan and a random website selling pills is huge-and it can cost you hundreds of dollars if you don’t know the rules.
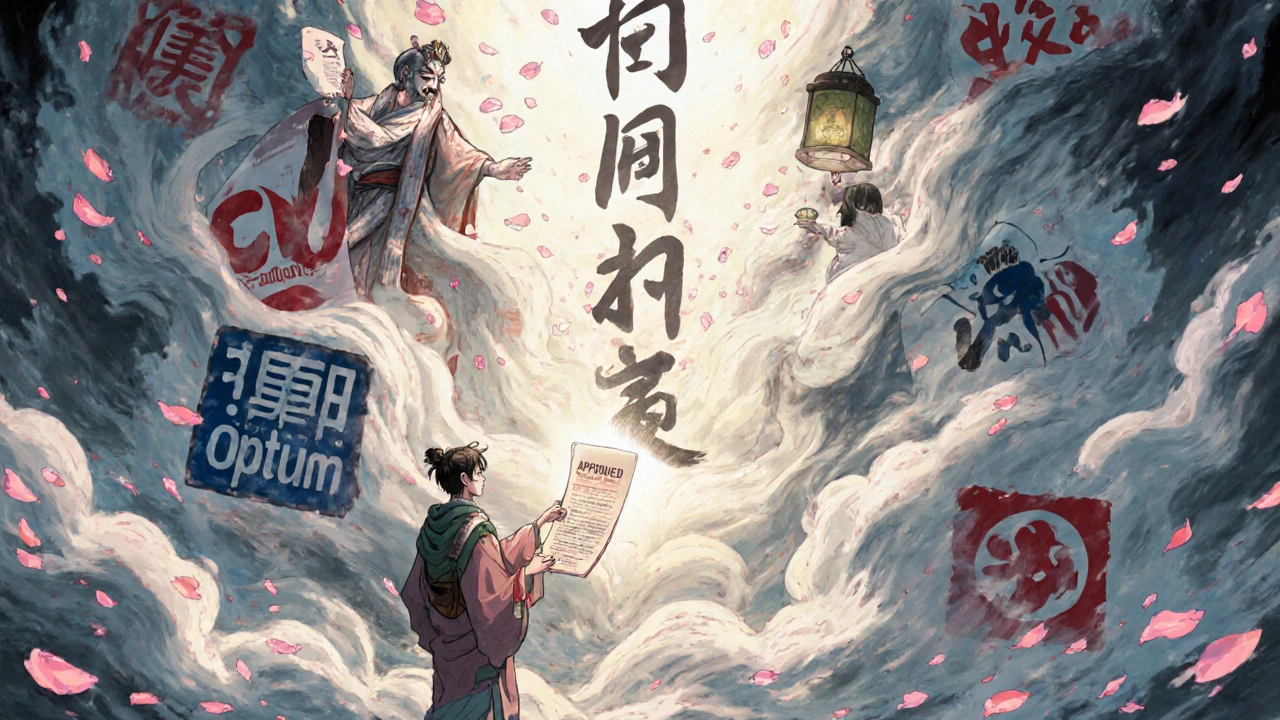
Your insurance doesn’t cover every online pharmacy. It only covers the ones that are part of its pharmacy network. These are usually managed by Pharmacy Benefit Managers (PBMs) like CVS Caremark, Express Scripts, or Optum Rx. These companies decide which drugs are covered, how much you pay, and which pharmacies you can use. Independent online pharmacies? Most don’t accept insurance at all. They might let you upload your card, but that’s often just for price comparison-you’ll pay upfront and file for reimbursement, if you even can.
Mail-Order vs. Independent Online Pharmacies: The Real Difference
Not all online pharmacies are the same. Mail-order pharmacies are built into your insurance plan. You get your 90-day supply of generics like metformin, lisinopril, or atorvastatin delivered to your door. Copays are low: often $5 for a 30-day supply or $10 for 90 days. Delivery takes about a week, so it’s not for emergencies. But for long-term meds? It’s one of the cheapest ways to fill prescriptions.
Independent online pharmacies-like those you find through Google ads or social media-are different. They’re online stores, not part of your insurance network. Some might say they accept insurance, but what they really mean is they’ll let you submit a claim after you pay full price. That’s risky. Many won’t process the claim correctly, or your insurer won’t recognize them as in-network. You could end up paying $100 for a drug that costs $12 with insurance.
Amazon Pharmacy’s RxPass is a middle ground. For $5 a month, Prime members get access to over 100 common generics. No copay per prescription. No insurance needed. But here’s the catch: only specific drugs are included. If your thyroid med or cholesterol pill isn’t on the list, you’re back to square one. And you still need a valid prescription.
How Your Insurance Tier System Works (And Why It Matters)
Every insurance plan puts drugs into tiers. Tier 1 is generics. Tier 2 is preferred brands. Tier 3 is non-preferred brands. And Tier 4 or 5? Specialty drugs. Generics are almost always in Tier 1. That means the lowest cost to you.
Here’s how it breaks down:
- Tier 1 (Generics): Fixed copay-usually $5 for 30 days, $10 for 90 days.
- Tier 2 (Preferred Brands): Coinsurance-30% of the plan’s allowed amount, capped at $200.
- Tier 3 (Non-Preferred Brands): Coinsurance-50% of allowed amount, capped at $200.
That’s why your insurer pushes generics. They save money-for them and for you. But here’s the twist: sometimes your doctor prescribes a brand-name drug, and your insurance forces you to switch to a generic-even if your doctor says no. This is called non-medical switching. It’s legal, common, and often happens without your knowledge. A 2023 survey found that 27% of insurance-related pharmacy calls were from people confused about why their medication changed.

What to Do When Your Insurance Forces a Generic Switch
If your insurance switches your brand drug to a generic without asking, and you have side effects, you’re not stuck. You can request a formulary exception. That means your doctor files paperwork saying why the generic won’t work for you. Maybe you had a bad reaction. Maybe your condition is unstable. Maybe the generic just doesn’t control your symptoms.
Insurers have to review these requests. They often approve them if your doctor provides clear medical reasons. But you have to ask. Don’t assume they’ll notice. Call your plan’s member services. Ask for a prior authorization form. Get your doctor to fill it out. It takes a few days, but it’s worth it.
Some plans even have 24/7 nurse lines. MHBP’s number is 1-800-556-1555. Nurses there can walk you through your formulary, explain why a drug was switched, and help you start the exception process. Use them. They’re free.
When It’s Cheaper to Skip Insurance Altogether
Here’s a surprise: sometimes paying cash is cheaper than using your insurance. Especially if you have a high-deductible plan. Walmart, Target, and Costco sell dozens of generics for $10 for a 90-day supply. That’s less than most insurance copays for the same drugs.
Check GoodRx or SingleCare before you use your insurance. Enter your drug, your dose, and your zip code. You’ll see cash prices side by side with your insurance copay. If the cash price is lower, pay cash. Your insurance doesn’t count cash purchases toward your deductible anyway, so you’re not losing anything.
One Reddit user shared: “I pay $10 for 90 days of metformin at Walmart. My insurance copay is $15. I stopped using insurance for it. Saved $78 a year.” That’s not rare. It’s common.
How to Check Coverage Before You Order
Don’t guess. Always verify. Here’s how:
- Find your plan’s drug list (formulary). Go to your insurer’s website and search for “formulary” or “drug list.”
- Enter the generic name of your drug. Make sure it’s listed and in Tier 1.
- Check if the online pharmacy you’re using is in-network. Look for a list of approved pharmacies.
- Use your insurer’s cost estimator tool. CVS Caremark, Express Scripts, and Aetna all have online drug cost checkers. Enter your drug, dose, and pharmacy.
- If it’s a third-party online pharmacy, call them. Ask: “Do you accept my insurance plan?” Then give them your plan name and member ID.
Pro tip: Write down the name of the pharmacist you talk to. If something goes wrong later, you’ll have a name to reference.
The Big Picture: Why This System Exists
Insurance companies don’t push generics because they’re evil. They push them because they work. Generics are just as safe and effective as brand-name drugs. They’re cheaper to make. And they save the system billions. In 2023, PBMs saved U.S. patients an estimated $320 billion by favoring generics.
But the system is complex. PBMs control 92% of prescription drug plans. The top three-CVS Caremark, Express Scripts, and Optum Rx-handle over 70% of all prescriptions. They decide what’s covered, what’s not, and how much you pay. And they’re under pressure to cut costs even more.
That’s why you’re seeing more mail-order use. In 2022, 32% of generic maintenance meds were filled through mail-order. By 2025, that’s expected to hit 45%. It’s more efficient. Fewer trips to the pharmacy. Lower distribution costs. Lower prices for you.
Still, the rise of Amazon RxPass and cash-price pharmacies shows people are looking for alternatives. The old system isn’t broken-it’s just being challenged.
What You Can Do Today
You don’t need to be a healthcare expert to save money on generics. Here’s your quick action plan:
- Know your plan’s formulary. Check it every time you refill.
- Use mail-order for maintenance drugs if your plan offers it. Save on copays.
- Compare cash prices with your insurance copay using GoodRx.
- If you’re switched to a generic and feel worse, ask for a formulary exception.
- Call your pharmacy before you order online. Ask: “Do you accept my insurance?”
- Use your insurer’s nurse line. It’s free and designed for exactly this kind of confusion.
Generic drugs are one of the best deals in healthcare. But you have to play the system right. Don’t let confusion cost you money. Know your options. Ask questions. Take control.
Do online pharmacies accept insurance?
Only if they’re part of your insurance plan’s pharmacy network. Most independent online pharmacies don’t accept insurance directly. They may let you submit a claim after paying, but reimbursement isn’t guaranteed. Always call the pharmacy and ask before ordering.
Is it cheaper to use insurance or pay cash for generics?
It depends. If you have a low-deductible plan, insurance copays ($5-$10) are usually cheaper. But if you have a high-deductible plan, cash prices at Walmart, Costco, or Target can be lower-sometimes $10 for 90 days. Always check GoodRx or SingleCare before using insurance.
Can my insurance force me to take a generic drug?
Yes. This is called non-medical switching. Insurers can require you to use a generic even if your doctor prescribes a brand-name drug. If you have side effects or your condition worsens, you can request a formulary exception. Your doctor must submit documentation supporting the need for the brand drug.
What’s the difference between mail-order and online pharmacies?
Mail-order pharmacies are part of your insurance plan’s network and require 90-day prescriptions. They’re managed by PBMs like Express Scripts and offer lower copays. Independent online pharmacies are third-party sellers. They may not accept insurance, and delivery times and drug quality vary. Always verify legitimacy before ordering.
Does Amazon Pharmacy accept insurance?
Amazon Pharmacy doesn’t bill insurance directly for most customers. Instead, it offers RxPass-a $5/month subscription for over 100 common generics. You can still use insurance for drugs not on RxPass, but you’ll pay the full price upfront and may get partial reimbursement. It’s not a replacement for traditional insurance coverage.
How do I know if my drug is covered by insurance?
Go to your insurer’s website and use their drug formulary search tool. Enter the generic name of your medication. Look for the tier and copay amount. If you’re unsure, call the number on your insurance card and ask for the pharmacy benefits department. They can confirm coverage and tell you which pharmacies are in-network.
What should I do if my insurance denies coverage for a generic?
If your insurance denies coverage, ask why. Sometimes it’s a simple error-like the drug name being misspelled. If it’s a formulary exclusion, your doctor can file a prior authorization or formulary exception. Keep records of all communication. If you’re denied, you can appeal. Most plans have a 60-day window to file an appeal.
Next Steps: How to Save on Your Next Generic Prescription
Start today. Open your insurance portal. Search for your most-used generic drug. Note the copay. Then open GoodRx. Type in the same drug. Compare prices. If cash is cheaper, pay cash. If mail-order is cheaper, ask your doctor for a 90-day prescription. If you’ve been switched to a generic and feel off, call your doctor and your insurer. Don’t wait until you’re in crisis.
Generic drugs save lives. But only if you can get them affordably. Know your plan. Know your options. You’re not powerless in this system-you just need to ask the right questions.






Just paid $8 for 90 days of lisinopril at Walmart. Insurance wanted $15. No brainer.
Y’all ever just feel like the system is designed to make you run in circles? I spent 45 minutes on the phone with my PBM last week because they switched my generic without telling me. My anxiety got worse. My doctor had to write a letter. They approved it. But why does it have to be this hard? I just want my meds to work, not play detective.
I get why people are frustrated, but let’s not forget-generics save lives. I’ve seen people skip doses because brand names cost $300. My cousin died because she couldn’t afford her insulin. Generics aren’t perfect, but they’re the reason millions aren’t choosing between food and medicine.
Let’s be clear: PBMs are not ‘healthcare providers’-they’re profit-driven middlemen who extract value from a broken system. They negotiate rebates with pharma, inflate list prices, and then tell you ‘your copay is $5’-but only if you use their network. Meanwhile, the actual cost of manufacturing metformin is less than $0.05 per pill. The system is a Ponzi scheme dressed in blue scrubs.
It is imperative to underscore that the structural integrity of the pharmaceutical benefit management ecosystem is predicated upon evidence-based formulary design and cost-containment protocols. While anecdotal experiences are emotionally compelling, they must be contextualized within the broader macroeconomic framework of healthcare delivery. The tiered formulary system, for instance, is not arbitrary-it is a calibrated mechanism designed to optimize therapeutic outcomes while minimizing systemic expenditure. Patients are not powerless; they are stakeholders with recourse through formal appeals processes, prior authorization requests, and utilization review channels. Proactive engagement with one’s plan administrator is not merely advisable-it is clinically and financially responsible.
Oh wow, so now we’re supposed to be grateful that our insurance forces us onto generics that make us feel like zombies? My doctor prescribed brand-name lamotrigine because the generic gave me migraines and brain fog. They switched me anyway. I had to go to the ER. Now I’m stuck paying cash for $120/month because ‘it’s not covered.’ And you call that ‘saving money’? Please. This isn’t healthcare. It’s a casino where the house always wins.
Big tip: If you’re on a high-deductible plan, always check GoodRx BEFORE you swipe your card. I saved $200 last month just by paying cash for my thyroid med. Also-Amazon RxPass is legit for the 100+ drugs they list. I get metformin, atorvastatin, and levothyroxine for $5/month. No insurance needed. But DO check the list-some meds are excluded. And yes, you still need a prescription. 😊
As a person who has navigated the American healthcare system for over a decade, including managing chronic conditions and dealing with multiple insurance providers across different states, I must emphasize that the complexity of insurance coverage for online pharmacies is not merely a matter of individual negligence but a systemic failure of transparency and standardization. The fact that one must call each pharmacy individually to verify network participation, cross-reference formularies across multiple platforms, and sometimes even engage in multi-day correspondence with customer service representatives to determine whether a $10 generic is covered under a $15 copay structure is not efficiency-it is bureaucratic exhaustion. Moreover, the rise of cash-price pharmacies and subscription models like RxPass reflects not just consumer ingenuity but a profound loss of trust in institutional healthcare intermediaries. The real question is not whether you should pay cash or use insurance-it is why, in the wealthiest nation on Earth, a person must become a part-time pharmacist, lawyer, and financial analyst just to afford a daily pill.
Look, I don’t care what the PBM says-America’s healthcare system is being gutted by foreign-owned corporations and corporate greed. I paid $3 for my blood pressure med at Costco last week. My insurance wanted $12. That’s not ‘savings’-that’s exploitation. We need to stop letting these middlemen take our money. Buy cash. Use Walmart. Support American-owned pharmacies. And stop trusting these big-name PBMs-they’re not your friends. They’re the reason your meds cost more than your rent.