Antihistamine Driving Safety Checker
Check Your Medication Safety
See if your antihistamine is safe for driving based on scientific evidence from 100+ studies.
Enter your antihistamine details to see if it's safe for driving.
Driving After Taking Antihistamines: A Hidden Danger
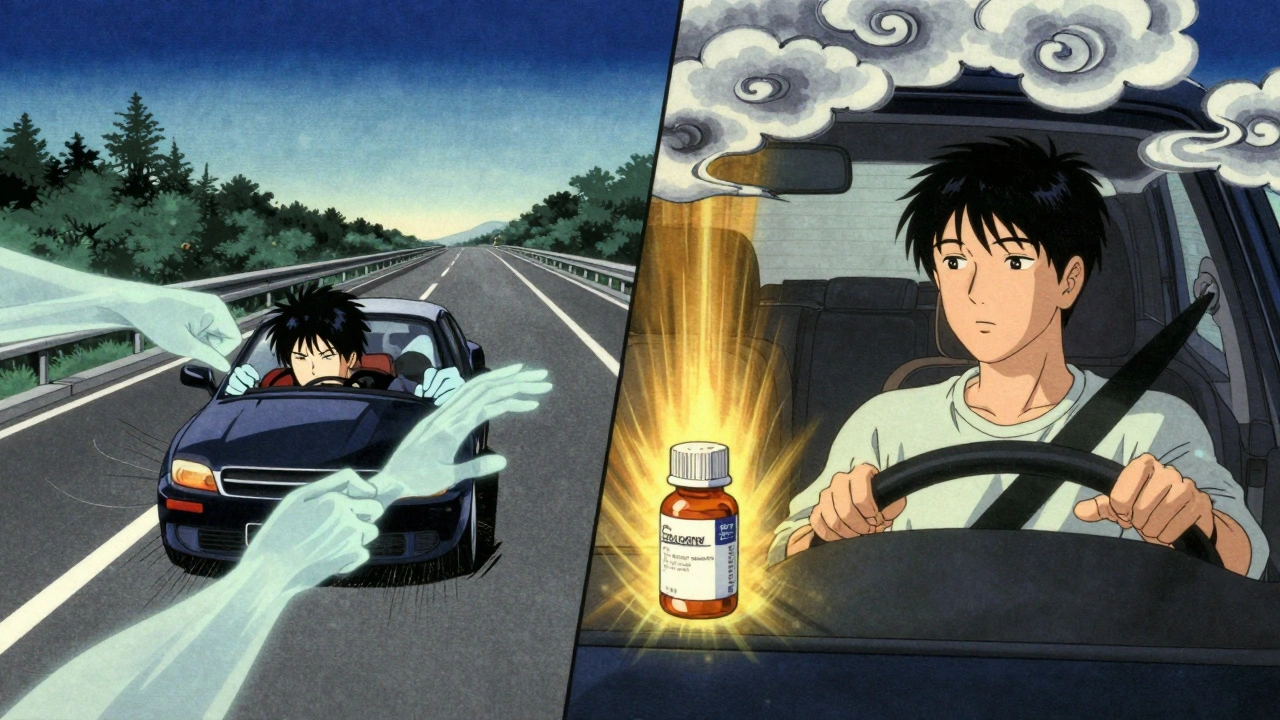
It’s 7 a.m. You’ve got allergies, so you pop a Benadryl before heading to work. You feel fine. No drowsiness. So you drive. But your reaction time is slower. Your focus is off. You almost missed the stop sign. You didn’t feel it, but your brain was still affected. This isn’t rare. It happens every day-and it’s one of the most overlooked risks on the road.
First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and clemastine are designed to block histamine to stop sneezing and runny noses. But they also cross into your brain, slowing down your central nervous system. That’s why they make you sleepy. And that’s why they make you a dangerous driver-even if you don’t feel it.
Not All Antihistamines Are the Same
There are three generations of antihistamines, and the difference between them isn’t just marketing. It’s life or death on the road.
First-generation antihistamines-like diphenhydramine, hydroxyzine, and dexchlorpheniramine-are the old-school options. They’re cheap, widely available, and often found in sleep aids and cold medicines. But they’re also the most likely to impair driving. Studies show they cause lane deviation equal to a blood alcohol level of 0.05-0.08%. That’s the legal limit in most places. Even worse, they linger in your system. Diphenhydramine has a half-life of 4 to 12 hours. So that morning pill? It could still be affecting you at 8 p.m.
Second-generation antihistamines-like cetirizine (Zyrtec) and loratadine (Claritin)-were made to be less sedating. But they’re not risk-free. Cetirizine, even at the standard 10mg dose, causes measurable impairment in 15-20% of users. Loratadine is generally safer, but not for everyone. Some people still feel foggy. And if you take a double dose? Impairment spikes.
Third-generation antihistamines-fexofenadine (Allegra) and levocetirizine (Xyzal)-are the gold standard for drivers. They barely enter the brain. Multiple double-blind, on-the-road driving studies show no significant difference between these drugs and placebo. No increased lane weaving. No slower reaction times. No higher crash risk. If you drive regularly and have allergies, these are the only ones you should be taking.
What the Science Says About Driving Impairment
Over 100 studies have tested how antihistamines affect driving. The results are clear and consistent.
First-generation antihistamines reduce reaction time by up to 30%. They make it harder to track moving objects, maintain speed, and respond to sudden changes. In one study, drivers on diphenhydramine were six times more likely to be involved in a crash than those on placebo. That’s worse than texting while driving, which quadruples crash risk.
Even when people say they feel fine, they’re often wrong. Research shows 70% of users can’t accurately judge their own impairment after taking sedating antihistamines. You might think you’re alert, but your brain is still sluggish. That’s why experts recommend a 48-hour test period at home before driving after starting any new antihistamine. Start with simple tasks. Then try a quiet, low-traffic drive. Don’t assume you’re okay just because you didn’t fall asleep.
Alcohol + Antihistamines = A Deadly Mix
Drinking one beer after taking Benadryl doesn’t just make you sleepy. It multiplies the danger.
Combining first-generation antihistamines with alcohol increases driving impairment by 200-300%. That’s not a guess. It’s measured in lab tests. The two substances work together to slow brain activity. Your coordination tanks. Your judgment disappears. You might not even realize how impaired you are-until it’s too late.
And it’s not just alcohol. Other sedatives, painkillers, muscle relaxants, and even some herbal sleep aids can have the same effect. If you’re on any medication, check the label. If it says “may cause drowsiness,” don’t mix it with antihistamines.
Real People, Real Consequences
Reddit threads and user surveys tell stories that studies can’t fully capture.
In a 2022 thread on r/Allergies, 63% of respondents admitted to feeling drowsy or slowed down while driving after taking first-gen antihistamines. Twelve percent said they had near-miss crashes or had to pull over because they couldn’t stay awake. One user wrote: “Took Benadryl before a road trip and had to pull over three times because I kept nodding off-never doing that again.”
On the flip side, 82% of users on fexofenadine reported no impact on driving. That’s not luck. That’s science. But even then, 18% said they felt slightly slower during heavy traffic or complex maneuvers. That’s why it’s still smart to test any new medication at home first.
Legal Risks You Can’t Ignore
Driving under the influence of impairing medication isn’t just dangerous-it’s illegal.
In 22 European countries, it’s against the law to drive within 8-12 hours of taking first-generation antihistamines. In 14 countries, these drugs are classified as controlled substances, and driving while using them can lead to fines, license suspension, or even criminal charges.
In the U.S., while there’s no federal law specifically banning antihistamine use while driving, you can still be charged with DUI if an officer determines your driving was impaired by medication. Police don’t need a breathalyzer to prove impairment. They use field sobriety tests. And if you’re in an accident, toxicology screens will reveal what you took. Insurance companies may deny claims if they find you were driving under the influence of a known sedative.
And here’s the kicker: Over-the-counter labels often don’t warn you clearly. Prescription labels do. But if you’re buying Benadryl at the gas station, the warning might be buried in tiny print. Don’t rely on the label. Know what you’re taking.
What You Should Do Instead
If you drive and have allergies, here’s your simple action plan:
- Switch to fexofenadine or levocetirizine. These are the only antihistamines proven safe for drivers. They work just as well as the old ones, without the drowsiness.
- Avoid first-gen antihistamines entirely. That means no Benadryl, no Unisom, no generic sleep aids unless they’re labeled as “non-drowsy.” And even then, check the active ingredient.
- Don’t take any antihistamine right before driving. Even safe ones can affect you differently on an empty stomach or if you’re tired. Take them at night instead.
- Test new meds at home. Try your new antihistamine on a weekend. Do a few chores. Sit in the driver’s seat. See how you feel. Don’t rush into driving.
- Never mix with alcohol or other sedatives. That’s not a gray area. It’s a red flag.

Why Cost Shouldn’t Be Your Guide
First-generation antihistamines cost about $4 a month. Fexofenadine runs $35. That’s a big difference.
But here’s what you’re really paying for: the cost of a crash. Medical bills. Lost wages. Legal fees. Higher insurance premiums. And worst of all-life-altering injury or death.
Insurance companies estimate that widespread use of third-generation antihistamines could cut medication-related crashes by 40-50% over the next decade. That’s thousands of lives saved. And it starts with one simple choice: switching to a safer option.
What’s Changing in 2025
The medical community is catching up. In 2023, the European Medicines Agency updated guidelines requiring all antihistamine labels to clearly state driving risks based on drug generation. The American Medical Association now recommends screening for antihistamine use during driver’s license medical exams for high-risk groups.
New drugs are coming. Levocabastine nasal spray, approved in 2021, shows no driving impairment in clinical trials. Seven more third-generation candidates are in late-stage testing.
But the biggest change? Awareness. More doctors are prescribing fexofenadine and levocetirizine as first-line treatment for drivers. And more patients are asking for them.
Final Takeaway: Your Safety Is Worth the Cost
Antihistamines don’t have to slow you down. You don’t have to choose between allergy relief and safe driving. The science is settled. The options are clear. And the consequences of ignoring them are too real to risk.
If you drive, and you take antihistamines, stop guessing. Stop hoping you’re fine. Switch to fexofenadine or levocetirizine. Take them at night. Avoid alcohol. And never assume you’re alert just because you didn’t fall asleep.
Driving safely isn’t about willpower. It’s about choosing the right medicine. And that choice could save your life-or someone else’s.





Fexofenadine for life. No drowsiness. No drama. Just clear skies and clear thinking behind the wheel.
You people still take Benadryl like it’s candy? Bro, you’re not ‘fine’-you’re just in denial. That stuff slows your CNS like a 2003 Nokia with a 12% battery. You’re a walking DUI waiting to happen. And don’t even get me started on the ‘I didn’t fall asleep’ excuse. 70% of users can’t even *perceive* their impairment. 🤦♂️
So let me get this straight… I’m supposed to pay $35 for a pill that doesn’t make me feel like a zombie, but I can get the zombie pill for $4? Oh wait-I’m supposed to *value my life* over my wallet? How radical. 🙄
This is such a needed post. Seriously. So many people don’t realize how dangerous this is. Switching to Allegra changed my life. I drive 40 miles to work every day and finally feel like myself again. You got this.
I took Zyrtec once before a road trip and felt like my brain was wrapped in cotton. I pulled over just to stare at a tree for 10 minutes. Not cool. Not okay. I switched to fexofenadine and now I’m actually awake during my commute. Thank god for science.
The deeper issue here isn’t just pharmacology-it’s the cultural normalization of self-medicated impairment. We’ve normalized the idea that if you don’t *feel* asleep, you’re not impaired. But cognition isn’t subjective. Reaction time, visual tracking, decision latency-these are measurable, objective functions. When you ingest a CNS depressant, you’re not ‘just being careful.’ You’re altering your neurochemistry. And the fact that we treat this like a personal choice rather than a public health hazard speaks volumes about how little we value systemic safety over individual convenience.
bro i used to take diphenhydramine all the time like its no big deal until i almost hit a kid on a bike. i wasnt even sleepy just kinda slow. now i only take allegra. its worth the extra bucks. peace.
The empirical data is unambiguous: first-generation H1 antagonists exhibit significant blood-brain barrier permeability, resulting in quantifiable decrements in psychomotor performance metrics including choice reaction time, divided attention, and lane-keeping accuracy. The pharmacokinetic profile of diphenhydramine-characterized by a prolonged half-life and active metabolites-further exacerbates residual impairment. Ergo, the clinical recommendation for third-generation agents is not merely prudent-it is bioethically imperative.
I can’t believe this is even a conversation. We live in a country where you can buy a 12-pack of Benadryl next to the chips and soda, but you need a 10-page form to get a vape. We’re literally prioritizing convenience over human life. And the worst part? The companies know. They make the dangerous stuff cheaper because they know people are lazy. I’m so done.
I appreciate the thoroughness of this post. The data is compelling, the distinctions between generations are clearly delineated, and the legal implications are underappreciated by the general public. That said, I would like to offer a nuance: individual metabolic variation is significant. While fexofenadine is statistically safer, there are rare cases where even third-generation agents induce mild sedation due to CYP3A4 polymorphisms or concurrent medication interactions. Therefore, while population-level recommendations are sound, personalized medical guidance remains essential. Still, for the vast majority, the shift to non-sedating agents is not just advisable-it is non-negotiable.
This is the kind of post that makes me feel less alone. I used to feel guilty for not being able to drive after taking my allergy meds… until I realized it wasn’t me, it was the medicine. Now I take my fexofenadine at night and wake up with zero fog. You’re not weak for needing this. You’re smart.