When you hear the word obesity, what comes to mind? Maybe diets that didn’t work, gym memberships that gathered dust, or well-meaning advice like "just eat less and move more." But what if losing weight isn’t about willpower? What if it’s a medical condition-like high blood pressure or diabetes-that needs the same kind of structured, ongoing care?
Medical weight management is no longer a fringe option. It’s a science-backed, clinically proven approach to treating obesity as a chronic disease. And in 2025, it’s more accessible, more effective, and more understood than ever before. This isn’t about quick fixes. It’s about long-term health: lowering your risk of heart disease, reversing type 2 diabetes, and improving your daily life.
What Exactly Is Medical Weight Management?
Medical weight management is a structured, team-based approach to treating obesity. It’s not just a prescription pill or a diet plan. It combines four key elements: medical supervision, nutrition therapy, behavioral counseling, and FDA-approved medications-all tailored to your body, your health, and your life.
The American College of Cardiology’s 2025 guidelines made it official: obesity is a chronic disease. That means it needs ongoing treatment, not just a one-time intervention. Clinics now use specific criteria to determine who qualifies. If your BMI is 30 or higher, you’re eligible. If it’s 27 or higher and you have conditions like high blood pressure, sleep apnea, or prediabetes, you’re still a candidate.
Unlike commercial weight loss programs that promise 20 pounds in 30 days, medical clinics focus on sustainable results. The goal? Lose at least 5% of your body weight. That’s not just a number-it’s the threshold where real health improvements start. Losing 5% can lower your blood pressure, improve insulin sensitivity, and reduce liver fat. Lose 10% or more? That’s when you might see type 2 diabetes go into remission.
How Do Medical Weight Management Clinics Work?
These aren’t your average wellness centers. They’re run by physicians, dietitians, and behavioral coaches who specialize in obesity. Most clinics follow a clear process:
- You start with a BMI check and medical review.
- You complete an orientation-sometimes a video, sometimes a booklet-that explains how the program works.
- You fill out detailed questionnaires about your eating habits, sleep, stress, and past attempts at weight loss.
- You get a personalized plan that includes nutrition, movement, and possibly medication.
At West Virginia University’s program, patients can’t even schedule their first appointment until they’ve watched the orientation and finished the pre-visit survey. That might sound strict, but it works. Patients who complete these steps are 60% more likely to stick with the program long-term.
Appointments are frequent at first. You’ll meet with a dietitian every 2 to 4 weeks for 30-minute sessions. These aren’t generic meal plans. They’re built around your food preferences, budget, and schedule. One patient might need help eating more vegetables because they work late. Another might need strategies to avoid late-night snacking after stress.
Behavioral coaching is just as important. Many people don’t realize how much emotions, sleep, and daily routines affect their eating. A good clinic helps you identify triggers-not to blame you, but to give you tools to respond differently.
The Medications: What’s Actually Working in 2025?
Medication is no longer a last resort. It’s a core part of treatment. The two most powerful drugs right now are semaglutide (Wegovy®) and tirzepatide (Zepbound®). Both are GLP-1 receptor agonists-medications originally developed for type 2 diabetes that turned out to be incredibly effective for weight loss.
Here’s what the numbers show:
- Semaglutide (2.4 mg weekly): Average weight loss of 14.9% over 72 weeks.
- Tirzepatide (15 mg weekly): Average weight loss of 20.2% over 72 weeks.
Tirzepatide is slightly more effective, but it’s also newer and harder to get. Insurance coverage for these drugs is still patchy. Only 68% of commercial insurers cover them in 2025-compared to 98% coverage for diabetes medications. Medicare Advantage plans cover them in just 12% of cases.
There’s also retatrutide, a new triple agonist (targeting GLP-1, GIP, and glucagon) showing 24.2% average weight loss in early trials. It’s not FDA-approved yet, but it’s coming fast.
These aren’t magic pills. They work best when paired with lifestyle changes. One study found that people who took semaglutide but didn’t change their diet lost half as much weight as those who combined it with nutrition counseling.
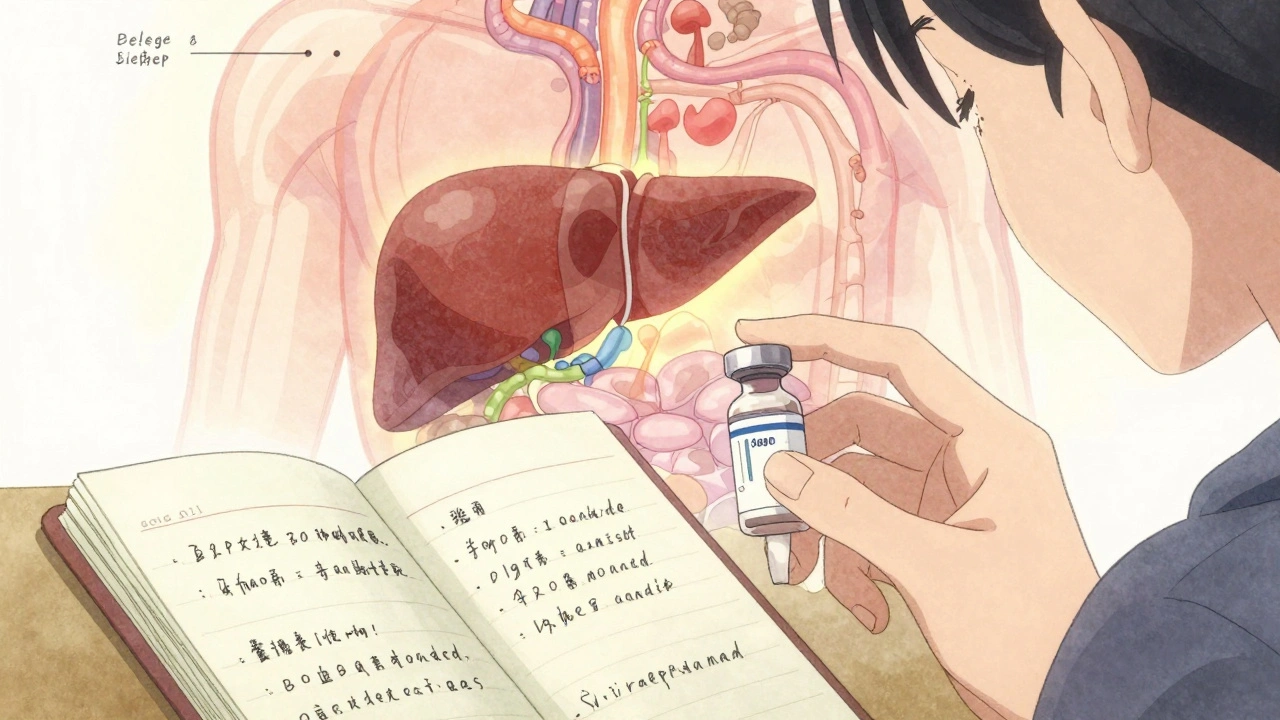
Monitoring: It’s Not Just About the Scale
Medical weight management isn’t just about how much you weigh. It’s about what’s happening inside your body.
At every visit, your provider checks:
- Waist circumference (a better predictor of heart risk than BMI)
- Blood pressure
- Liver enzymes
- Cholesterol and blood sugar levels
- Medication side effects (nausea, fatigue, constipation)
The American Diabetes Association recommends checking these metrics at least every 3 months during active treatment. That’s because improvements happen fast. One patient saw their A1C drop from 7.8% to 5.9% in just 5 months after starting tirzepatide and adjusting their meals.
Many clinics now use electronic health record templates to track obesity-related data consistently. That means your weight, lab results, and progress notes are all in one place-so your doctor can spot trends and adjust your plan before things go off track.
Clinics vs. Commercial Programs: The Real Difference
Let’s say you’re comparing a medical clinic to a popular online weight loss app. The clinic might cost $200 a month. The app? $40.
But here’s what the data shows:
| Factor | Medical Weight Management | Commercial Programs |
|---|---|---|
| Average 12-month weight loss | 9.2% | 5.1% |
| Retention rate after 1 year | 68% | 32% |
| Insurance coverage | Partial (varies) | None |
| Medical supervision | Yes | No |
| Medication access | Yes | No |
| Personalized nutrition plans | Yes (by registered dietitian) | Generic templates |
The higher cost of medical clinics pays off. Patients in these programs are more likely to keep the weight off. They’re also less likely to develop complications like heart attacks or kidney disease down the road.
And here’s something surprising: the safety profile is better than bariatric surgery. Complication rates for medical weight management are around 0.2%. For gastric bypass? 4.7%.
Who Gets Left Behind?
Despite all the progress, big gaps remain. Black and Hispanic patients are 43% less likely to be offered weight-loss medications-even when they meet the same BMI and health criteria as white patients. That’s not a coincidence. It’s systemic bias.
Some clinics still use language that blames patients: "You didn’t try hard enough." The ACC’s 2025 guidelines explicitly warn against this. They recommend using neutral language: "Let’s talk about what’s been working and what hasn’t." They also suggest practical changes: chairs without armrests, blood pressure cuffs in multiple sizes, and waiting rooms that don’t feel like a judgment zone.
Cost is another barrier. Even with insurance, co-pays for tirzepatide can hit $500 a month. Some patients wait 3 to 8 weeks just to get approval. That delay costs them momentum-and sometimes, their health.
But things are changing. Forty-seven percent of Fortune 500 companies now offer medical weight management as part of employee wellness programs. That’s up from 18% in 2022. More employers are seeing the return on investment: every dollar spent on these programs saves $2.87 in future healthcare costs for diabetes and heart disease.
What Does Success Look Like?
Success isn’t a size 6 or a flat stomach. It’s:
- Needing fewer medications for high blood pressure.
- Being able to walk up the stairs without stopping.
- Getting a good night’s sleep without a CPAP machine.
- Not feeling ashamed to see your doctor.
A 2025 survey by the Obesity Action Coalition found that 78% of people in medical weight management programs reported improved quality of life after 6 months. The top reasons? Personalized meal plans and a non-judgmental team.
One woman in Adelaide, 52, lost 18% of her body weight over a year. She didn’t run marathons. She didn’t cut out carbs completely. She started walking 20 minutes after dinner. She swapped soda for sparkling water. She got on tirzepatide after her doctor explained it wasn’t a failure-it was a tool. Now, her A1C is normal. She’s off her blood pressure pill. And she says, "I finally feel like I’m in control. Not because I’m strong. Because I got the right help."
Where Do You Start?
If you’re considering medical weight management:
- Check your BMI. If it’s 30 or higher, or 27+ with a related condition, you qualify.
- Ask your doctor if they offer or refer to a medical weight management program.
- Call local clinics. Ask: "Do you use the ACC 2025 guidelines? Do you have dietitians and behavioral coaches on staff?" If they say "We just give out diet plans," move on.
- Check your insurance coverage for GLP-1 medications. If it’s denied, ask for a prior authorization appeal. Many approvals come through on appeal.
- Start with small goals. Lose 5%. Then 10%. Celebrate every step.
This isn’t about perfection. It’s about progress. And with the right support, it’s possible-for anyone, at any age, at any starting point.
Is medical weight management only for people with severe obesity?
No. Medical weight management is for anyone with a BMI of 30 or higher, or a BMI of 27 or higher with conditions like high blood pressure, type 2 diabetes, or sleep apnea. Even people with moderate weight loss goals benefit from the structured support, medication options, and health monitoring these clinics provide.
Do I have to take medication to join a medical weight management program?
No. Medication is one tool, not a requirement. Many people start with nutrition counseling, behavioral coaching, and physical activity. Medication is added only if needed and if you’re a good candidate. Your provider will discuss options based on your health history, preferences, and insurance coverage.
How long does it take to see results?
Most people start seeing weight loss within the first 4 to 8 weeks. The biggest changes happen in the first 6 months. But the real goal isn’t just weight loss-it’s keeping it off. Programs that last 12 months or longer have the best long-term success rates. Health improvements like lower blood sugar or blood pressure often show up even before the scale moves significantly.
Are these programs covered by insurance?
Coverage varies. Most commercial insurers cover some aspects-like dietitian visits or behavioral therapy-but not always the medications. Medicare Part B covers intensive behavioral therapy for obesity, but only 12% of Medicare Advantage plans cover GLP-1 drugs. Always check with your insurer before starting. Many clinics help with prior authorization appeals.
Can I do this on my own without a clinic?
You can lose weight on your own-but the odds of keeping it off are much lower. Studies show people in medical programs lose nearly twice as much weight as those using commercial apps or self-guided diets. The support, monitoring, and access to proven medications make a real difference. Think of it like managing high blood pressure: you wouldn’t try to do it alone without a doctor’s guidance.
What if I’ve tried everything and failed before?
That’s exactly why medical weight management exists. Past failures aren’t a sign of weakness-they’re a sign that the approach didn’t match your needs. This isn’t about trying harder. It’s about trying differently. With personalized plans, medication, and a team that understands the biology of obesity, many people who thought they’d never succeed find real, lasting results.


Oh honey, let me tell you-this isn't just medicine, it's *performance art* for the metabolic elite. Semaglutide? More like the Chanel No. 5 of weight loss-expensive, glamorous, and only for those who can afford to be seen holding the vial at brunch. Meanwhile, my cousin in Des Moines is still eating ramen and praying to the Scale Gods. The real tragedy? We’ve turned compassion into a luxury SKU.
It’s fascinating how we’ve rebranded willpower as a pharmacological intervention, isn’t it? The neoliberalization of the body-where metabolic dysfunction is commodified into GLP-1 agonism. We’ve moved from ‘eat less’ to ‘inject less’… but the underlying ethos remains the same: the body must be optimized. 🤔
Just read this and had to pause. The 5% weight loss threshold is such a critical marker-biologically, it’s when adipokine signaling starts shifting, inflammation drops, hepatic insulin sensitivity improves. It’s not just ‘feeling better’-it’s cellular recalibration. And the fact that clinics are tracking waist circumference and liver enzymes? That’s precision medicine. Kudos to the teams doing this right.
STOP. Just STOP. They’re giving people INJECTIONS to fix what they should fix by CHOOSING to eat better?! This is the exact reason America is broken. No one needs a $500-a-month shot to stop eating donuts. It’s moral decay. You don’t need a doctor to say ‘no’ to cake-you need a spine. And now we’re medicating weakness? I’m disgusted.
man i just want to say… this is actually kinda beautiful. like, imagine if we treated high blood pressure like this? no one would say ‘just stop being hypertensive’ right? so why do we treat fat like a character flaw? 🤍 maybe it’s not about discipline… maybe it’s about biology. and if science gives us tools? why not use ‘em? 🙏
Interesting how the retention rates are so much higher in medical programs. That tells me the structure matters more than the pill. The accountability, the consistency, the human connection-those are the real active ingredients. Medications help, sure, but without the weekly check-in with the dietitian? Most people fall back. It’s the rhythm that sustains.
Let’s not romanticize this. The 20.2% average weight loss with tirzepatide? That’s statistically significant, yes-but it’s not a population-level solution. It’s a boutique intervention for the insured, the educated, the white-collar. Meanwhile, Medicaid recipients are still being told to ‘walk more’ while their neighborhood has zero grocery stores and 17 fast food joints. This isn’t equity. It’s medical gentrification.
I’m from rural Kentucky. No clinic nearby. My doctor says ‘try yoga.’ I work two jobs. I don’t have time for 30-minute sessions. This sounds nice. But for most people? It’s a fantasy.
so many people here talking about pills like its magic… but what about the food? the stress? the sleep? i think the real problem is we live in a world that makes healthy choices hard. not that people are weak. just… tired. 🤷♂️
Big Pharma’s latest scam. They made obesity a disease so they could sell more drugs. You think they care about your health? They care about your insurance card. Wake up.
I’ve been thinking about this a lot lately-what if the real illness isn’t obesity, but the shame we’ve attached to it? The clinics that use neutral language, the chairs without armrests, the non-judgmental coaches… that’s the healing. The medication just helps the body catch up. The dignity? That’s what changes lives.
The data on long-term retention is compelling, but I wonder about the psychological burden of constant monitoring. Are we replacing one form of control (diet culture) with another (clinical surveillance)? The metrics are useful, but at what cost to mental autonomy? I’m not against treatment-I’m wary of the infrastructure.
There’s something deeply human in how this approach treats weight loss like chronic illness management-because it is. It’s not about willpower, it’s about systems. And the fact that employers are starting to invest? That’s the real shift. When the cost of inaction becomes clearer than the cost of care, change happens. Slowly, yes. But it’s happening.
Look, I used to think this stuff was overhyped. Then I watched my sister go through it-no magic, no drama, just a team that showed up every week. She lost 18%, got off her BP meds, and now she hikes with her grandkids. That’s not a pill. That’s love wrapped in science. And yeah, it costs money-but so does a heart attack. Choose your investment.