Drinking a glass of pomegranate juice might feel like a healthy choice-rich in antioxidants, sweet, and full of vitamins. But if you’re taking medication, especially for heart conditions, blood thinning, or mental health, that glass could be more risky than you think. The problem isn’t the juice itself. It’s what it does inside your body when it meets your pills.
How Pomegranate Juice Interacts With Your Medications
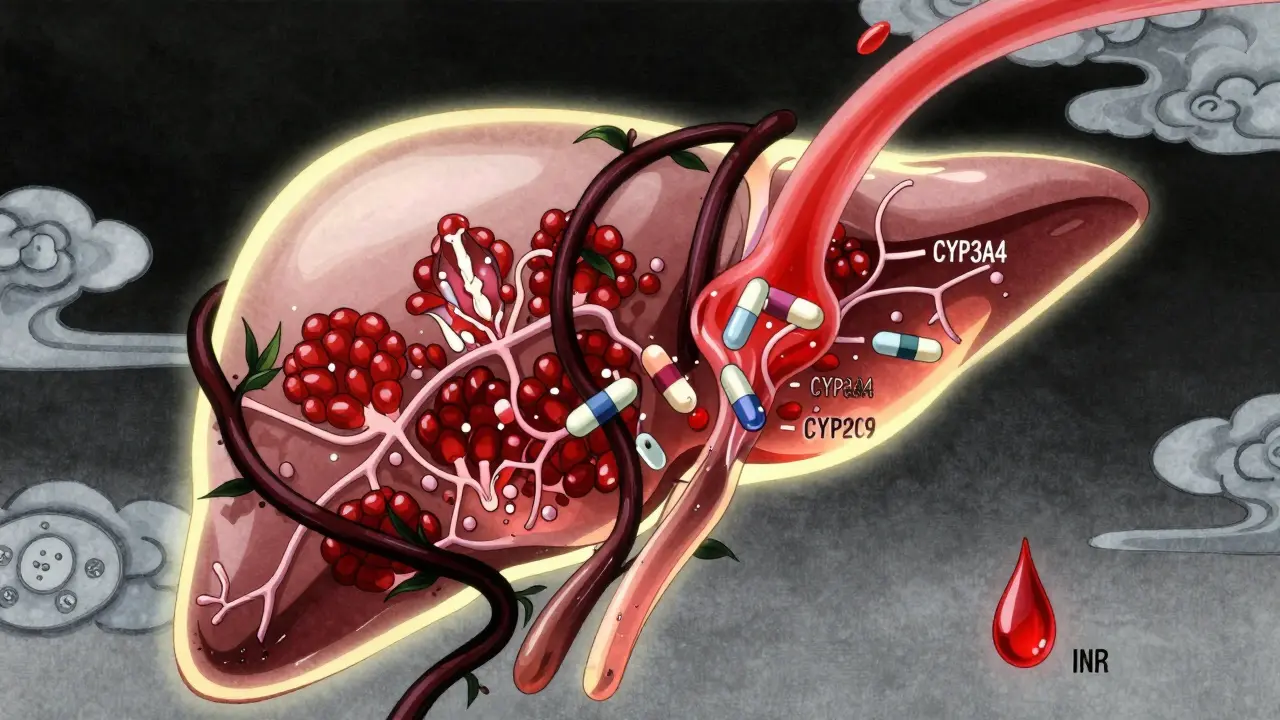
Pomegranate juice doesn’t just sit in your stomach. It gets absorbed into your bloodstream and starts interacting with enzymes in your liver and intestines. These enzymes-called CYP3A4 and CYP2C9-are responsible for breaking down about 60% of the medications people take daily. When pomegranate juice blocks these enzymes, your body can’t process the drugs the way it should.This means more of the drug stays in your system. For some medications, that’s harmless. For others, it’s dangerous. Think of it like pouring extra fuel into a car engine that wasn’t designed for it. The engine might sputter, stall, or even catch fire. With medications, the result can be too much drug in your blood, leading to side effects or toxicity.
One of the most studied interactions is with warfarin, a blood thinner used to prevent clots. Warfarin has a very narrow window between working and causing harm. Too little, and you risk a stroke or clot. Too much, and you could bleed internally. Studies show that pomegranate juice can raise INR levels-the measure of how long your blood takes to clot-by 0.5 to 1.5 units in some people. One case reported in the Pharmaceutical Journal showed INR jumping from 2.5 to 4.1 after just a few days of daily pomegranate juice. That’s enough to put someone at serious risk of bleeding.
Not All Medications Are Affected the Same Way
It’s easy to assume that if pomegranate juice affects one drug, it affects them all. But that’s not true. The interaction depends on three things: the specific enzyme the drug uses, how much of the drug is processed by that enzyme, and how sensitive the drug is to small changes in blood levels.Drugs that rely heavily on CYP3A4 or CYP2C9 are the ones to watch. These include:
- Statins like atorvastatin (Lipitor) and simvastatin (Zocor)-used to lower cholesterol. Too much can cause muscle damage.
- Antidepressants such as sertraline and quetiapine-can lead to dizziness, low blood pressure, or serotonin syndrome.
- ACE inhibitors like lisinopril and enalapril-used for high blood pressure. Pomegranate juice may amplify their effect, causing blood pressure to drop too low.
- Immunosuppressants like cyclosporine-critical for transplant patients. Even small increases can be toxic.
- Benzodiazepines such as midazolam-used for anxiety or sedation. Higher levels can cause excessive drowsiness or breathing problems.
On the flip side, many common medications-like ibuprofen, metformin, or levothyroxine-don’t rely on these enzymes. For those, pomegranate juice is unlikely to cause trouble. The key is knowing which category your medication falls into.
Why Lab Results Don’t Always Match Real Life
You might have heard that pomegranate juice inhibits CYP3A4 by up to 50% in test tubes. That sounds alarming. But here’s the catch: what happens in a lab dish doesn’t always happen in your body.A 2014 study with 12 healthy volunteers found that drinking 330 mL of pomegranate juice daily for two weeks had no measurable effect on midazolam levels. The blood concentrations stayed almost exactly the same as when they didn’t drink the juice. Similar results showed up in studies with theophylline, a drug for asthma.
So why the contradiction? For one, the concentration of active compounds in juice varies wildly depending on the fruit, how it’s processed, and whether it’s pasteurized. A bottle from the store isn’t the same as the concentrated extract used in a lab. Also, your body absorbs and processes these compounds differently than a test tube. Some people’s enzymes are more sensitive. Others barely notice the effect.
This is why the FDA hasn’t issued a warning about pomegranate juice like it has for grapefruit juice. Grapefruit can increase statin levels by up to 15-fold. Pomegranate? The highest increase seen in humans is around 40%, and even that’s rare.
What Do Real People Experience?
Numbers don’t tell the whole story. Real people share their experiences online-and the results are mixed.On Reddit’s r/bloodthinners, 17 users reported INR spikes after starting pomegranate juice. One person had to cut their warfarin dose by 30% just to get their INR back to normal. Others saw no change at all.
On PatientsLikeMe, 214 people on warfarin who drank pomegranate juice regularly: 89% said their INR stayed stable. Only 11% noticed any fluctuation, and most of those were minor.
A 2022 survey of 1,247 people on long-term meds found that 28% drank pomegranate juice regularly. Only 4.7% reported any side effect that might have been linked to the juice. That’s a low rate-but still enough to warrant caution.
The takeaway? For most people, occasional or moderate use is fine. But if you’re on a medication with a narrow therapeutic window, don’t assume you’re in the safe 89%. You could be in the 11%.
What Experts Recommend
Major health organizations don’t tell you to stop drinking pomegranate juice. They tell you to be smart about it.The American Heart Association says: don’t quit cold turkey. Abruptly stopping something you’ve been drinking regularly can be just as risky as starting it. Consistency matters more than elimination.
Mayo Clinic advises: if you’re on warfarin, stick to no more than 8 ounces (about 240 mL) per day-and keep it the same every day. If you start or stop drinking it, get your INR checked within a week.
The University of North Carolina Pharmacy School suggests waiting at least two hours between taking your medication and drinking the juice. That gives your body time to absorb the drug before the juice hits your system.
The European Medicines Agency says the risk is low for most drugs-but for warfarin, they recommend closer monitoring during the first few weeks of adding pomegranate juice to your routine.
Bottom line: don’t panic. But don’t ignore it either.

What You Should Do Right Now
If you’re taking any prescription medication and you drink pomegranate juice, here’s what to do:- Check your meds. Look up your medication on a trusted drug interaction checker-like Mayo Clinic’s or WebMD’s. If it lists pomegranate juice as a moderate or major interaction, pay attention.
- Know your INR. If you’re on warfarin, keep track of your INR readings. If you notice unexplained spikes or drops after starting juice, tell your doctor.
- Be consistent. If you drink it, drink the same amount every day. Don’t binge one week and skip the next.
- Don’t self-diagnose. If you feel dizzy, unusually tired, bruise easily, or have unusual bleeding, don’t assume it’s the juice. Call your provider.
- Ask your pharmacist. They see drug interactions every day. Bring your juice bottle and your pill list. They’ll tell you if it’s a problem.
There’s no need to give up pomegranate juice unless your doctor says so. But treating it like a harmless smoothie is a mistake. It’s a bioactive substance. And like any substance that affects your body’s chemistry, it deserves respect.
What’s Next in Research?
Scientists are still trying to figure out who’s most at risk. A study funded by the National Institutes of Health is currently tracking 150 people taking 12 different medications while consuming pomegranate juice. Results aren’t due until late 2024, but early data suggest genetics might play a role. Some people have variations in their CYP2C9 or CYP3A4 genes that make them more sensitive to inhibition.Another study, led by the Pharmacogenomics Research Network, is looking at whether certain DNA markers predict who will have an interaction. That could one day lead to personalized advice: "Based on your genes, you can safely drink pomegranate juice. You? You should avoid it."
For now, the best advice is simple: know your meds, know your body, and talk to your healthcare team.
Can I drink pomegranate juice while taking warfarin?
You can, but with caution. Some people experience increases in INR, which raises bleeding risk. If you choose to drink it, stick to no more than 8 ounces per day, keep your intake consistent, and monitor your INR closely-especially when you start or stop. Always inform your doctor.
Is pomegranate juice as dangerous as grapefruit juice?
No. Grapefruit juice can increase blood levels of some drugs by up to 15 times. Pomegranate juice’s effect is much milder-usually under 40% increase, and often no effect at all in human studies. The FDA has issued strong warnings about grapefruit, but not pomegranate. That doesn’t mean pomegranate is harmless, just that the risk is lower and more variable.
Does cooking or pasteurizing pomegranate juice reduce the interaction risk?
Not significantly. The compounds that inhibit CYP enzymes-like punicalagins and ellagitannins-are stable under heat and pasteurization. Whether you drink fresh-squeezed, store-bought, or boiled-down concentrate, the risk remains similar. The key factor is the amount and frequency of consumption, not how it’s processed.
What if I only drink pomegranate juice once a week?
If you’re on a medication with a narrow therapeutic window (like warfarin, cyclosporine, or some statins), even occasional use can cause fluctuations. For most people, once a week is unlikely to cause problems. But if you’re unsure, check with your pharmacist or doctor. Consistency matters more than frequency.
Should I stop drinking pomegranate juice if I’m on multiple medications?
Not necessarily. Most medications aren’t affected. But if you’re taking any drug known to interact with CYP3A4 or CYP2C9-especially those with narrow therapeutic windows-it’s worth discussing. Don’t assume all your meds are safe just because one isn’t. Review your full list with your pharmacist.





I drink pomegranate juice every morning with my oatmeal. Never thought twice about it until I saw this post. My INR’s been stable for two years on warfarin. Maybe I’m just lucky? Or maybe my body doesn’t care.
Still, I’ll start tracking it now. Better safe than sorry.
Why are we even talking about this like it’s a crisis? You’re telling me some juice is gonna mess up my meds? Bro I drink grapefruit juice like water and I’m fine. This is just fearmongering dressed up as science.
In India, we use pomegranate in every festival. Juice, seeds, even paste. My uncle takes blood thinner for heart. He drinks it daily. No problem. Maybe it’s different for Americans? Or maybe doctors just scare people to sell more tests?
Let’s not pretend this is new. Pharmacists have been warning about CYP3A4 inhibitors since the 90s. Pomegranate isn’t the villain-it’s a symptom of how we treat food like medicine and medicine like candy. The real issue? We don’t educate patients. We just hand out scripts and hope for the best.
Also-yes, pasteurization doesn’t kill the punicalagins. But neither does boiling your tea. The dose makes the poison. Consistency matters more than fear.
This entire post is a textbook case of overmedicalization. 28% of people drink it. 4.7% report side effects. That’s less than a quarter of one percent of the population. Meanwhile, 70% of Americans are on at least one prescription. Should we ban all food? Or maybe-just maybe-people should stop being lazy and read their damn labels?
There’s a deeper philosophical question here: when does a natural substance become a drug? Pomegranate juice has no FDA approval, yet it alters enzyme kinetics with the precision of a pharmaceutical. We treat aspirin like a candy and pomegranate like a poison. But both are chemical agents. The difference? Profit motive. The pharmaceutical industry doesn’t own pomegranate farms.
I’ve been on cyclosporine since my kidney transplant 8 years ago. My doctor told me to avoid grapefruit. I didn’t know pomegranate was in the same category. I’ve been drinking it daily for 2 years. My levels are perfect. I cried when I read this. Not because I’m scared-but because I feel like I’ve been lied to by the system. Why didn’t anyone tell me? Why does this info feel buried?
My mom takes lisinopril and loves pomegranate. She drinks a glass every night. I asked her to stop after reading this. She said, 'I’ve been doing this for ten years and my BP is better than yours.' She’s 72. She knows her body better than any study. Maybe the real answer isn’t in the lab-it’s in listening to people?
I’m from Texas and I drink this stuff like it’s water 😍 I’ve got anxiety meds and a statin. Never had an issue. But I’m gonna start writing down my juice days and my mood days. Maybe there’s a pattern I didn’t see. 🤓✨ #healthawareness #pomegranatequeen
The data is messy because the human body is messy. Lab studies use concentrated extracts. Real people drink juice. Real people have gut microbiomes that vary. Real people sleep, eat, stress, and metabolize differently. We can’t reduce biology to a single enzyme pathway. This isn’t a warning-it’s a call for personalized medicine.
The notion that natural substances are inherently benign is a dangerous myth. The pharmacokinetic interference of pomegranate juice with CYP3A4 and CYP2C9 is well documented in peer-reviewed literature. While the magnitude of effect is often modest in vivo, the clinical implications for narrow therapeutic index agents are nontrivial. One must exercise prudent vigilance.
Oh here we go again. Another 'be careful with this fruit' panic. You know what’s really dangerous? The pharmaceutical industry selling you pills that cause liver failure, then telling you to avoid the one natural thing that might help your inflammation. Pomegranate juice doesn’t cause toxicity. The profit-driven medical-industrial complex does. They don’t want you to know that a $2 fruit might make your $200 pill less necessary. Don’t be fooled. This is corporate fear-mongering dressed in white coats.
In India we have a saying: 'What is medicine for one is poison for another.' This is true. My cousin had a bad reaction. My aunt drinks it daily and feels great. Maybe it’s genetics? Maybe it’s gut flora? Maybe it’s just luck? Science hasn’t figured it out yet. But we’ve been living with this for centuries. Don’t throw out the fruit. Just watch yourself.
I’m a nurse and I’ve seen this firsthand. A guy on simvastatin started drinking pomegranate juice every day. Three weeks later he couldn’t walk. Rhabdo. ICU. He didn’t know it could do that. His doctor didn’t tell him. So now I hand out a little card with every prescription: 'Avoid grapefruit, pomegranate, Seville oranges.' Simple. Clear. Saves lives.
just stop drinking the juice if ur on meds its not that hard