Warfarin & Antibiotic INR Calculator
Calculate INR Risk
Your Estimated INR After Antibiotic
Important: This is an estimate based on medical data. Actual results may vary. Always consult your doctor before changing medications.
INR Risk Levels
Safe
INR < 4.0
Typically no immediate bleeding risk. Monitor closely.
Caution
INR 4.0 - 5.0
Minor bleeding risk. Contact doctor.
Danger
INR 5.0 - 9.0
Major bleeding risk. Requires immediate medical attention.
Emergency
INR > 9.0
Life-threatening bleeding risk. Seek emergency care.
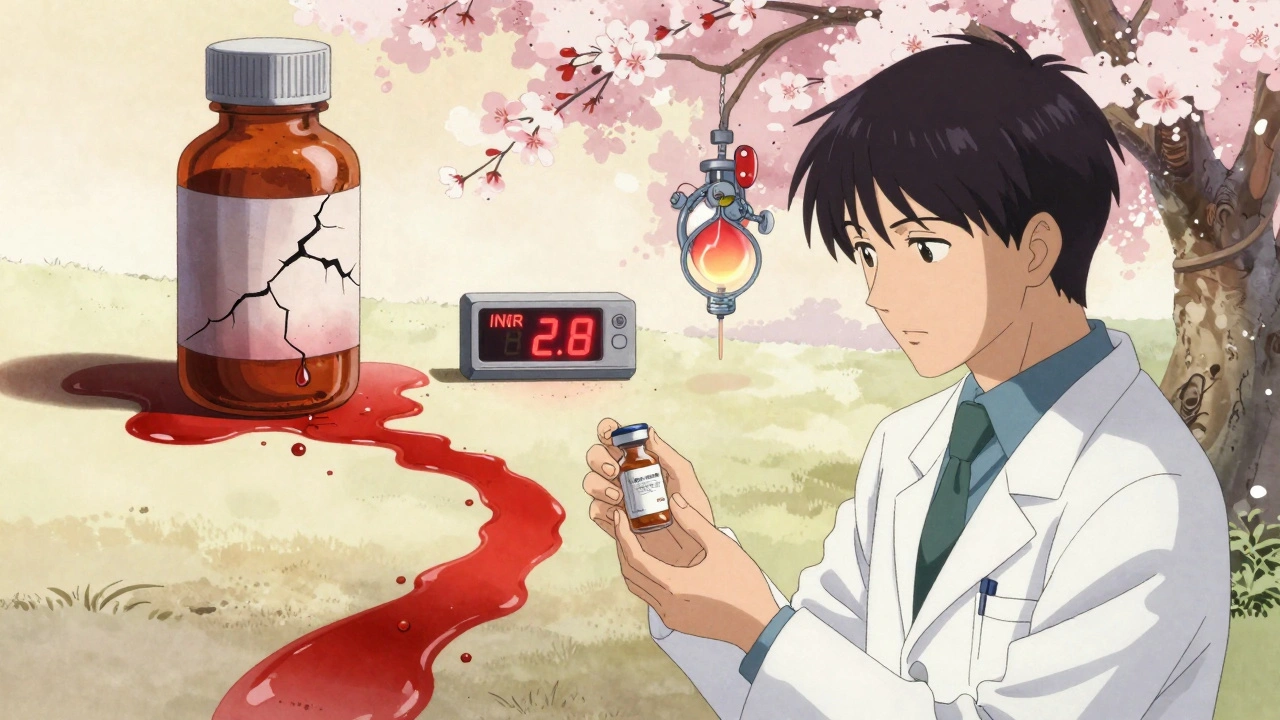
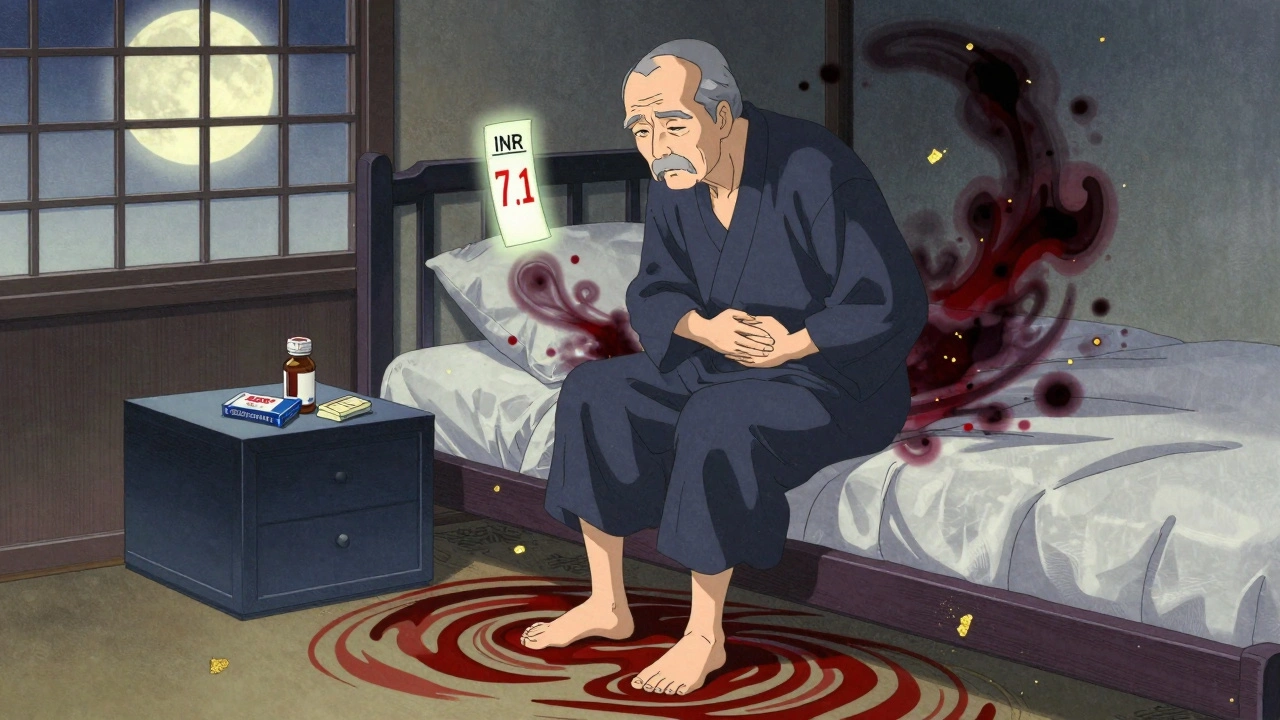
Imagine you’re on warfarin for a mechanical heart valve or atrial fibrillation. Your INR is steady at 2.8. You get a urinary tract infection. Your doctor prescribes trimethoprim-sulfamethoxazole - also known as Bactrim or Septra. Three days later, you feel dizzy. You check your INR at home. It’s 7.1. You’re bleeding internally. This isn’t rare. It happens more often than most people realize.
Why This Interaction Is So Dangerous
Warfarin doesn’t just thin your blood - it keeps your clotting factors in a tight balance. Too little, and you clot. Too much, and you bleed. Trimethoprim-sulfamethoxazole (TMP-SMX) throws that balance into chaos. The result? INR spikes. And when INR goes above 5.0, your risk of serious bleeding - like brain hemorrhage or gastrointestinal bleeding - jumps dramatically. This isn’t just theory. FDA data shows over 1,800 reports of INR elevation linked to TMP-SMX in just five years. Nearly half of those cases led to hospitalization. Almost 4% ended in death. The problem? Many doctors still prescribe it. And many patients don’t know to ask.How TMP-SMX Hijacks Warfarin
It’s not one mechanism - it’s three, working together. First, TMP-SMX blocks CYP2C9, the main liver enzyme that breaks down the most powerful part of warfarin: S-warfarin. Without this enzyme working, warfarin builds up. Studies show this alone can increase warfarin levels by 20-30%. Second, both drugs are highly bound to albumin in your blood. When TMP-SMX enters the system, it pushes warfarin off those protein sites. Now there’s more free warfarin floating around - active, unbound, and ready to thin your blood. Third, sulfamethoxazole wipes out good bacteria in your gut. Those bacteria make vitamin K. Less vitamin K means less clotting factor production. Warfarin already blocks vitamin K recycling. Now you’re double-whammied. The result? INR can climb from 2.5 to 6.0 in as little as 36 hours. That’s faster than most people realize.Not All Antibiotics Are Created Equal
If you’re on warfarin, not every antibiotic is a red flag. But TMP-SMX is one of the worst. Here’s what the data shows:- Trimethoprim-sulfamethoxazole: INR increases by an average of 1.8 units
- Ciprofloxacin (a fluoroquinolone): INR increases by 0.9 units
- Amoxicillin: INR increases by 0.4 units - barely noticeable
- Nitrofurantoin: No significant change - often the safest choice for UTIs

Who’s at Highest Risk?
This interaction doesn’t hit everyone the same way. Some people barely notice a bump. Others crash into danger. The biggest risk factors:- Age over 75 - liver and kidney function decline, so drugs stick around longer
- Heart failure - poor circulation slows drug clearance
- Liver disease - CYP2C9 activity drops
- Low vitamin K intake - from poor diet or malnutrition
- Male sex - men are 9% more likely to have dangerous INR spikes than women
What Happens When INR Spikes
You don’t always feel it. That’s the danger. An INR of 4.0-5.0? You might feel fine. But your body is one fall away from internal bleeding. Here’s what experts recommend:- INR 4.0-5.0, no bleeding: Skip 1-2 warfarin doses. Resume at 70-80% of your usual dose. Check INR again in 2-3 days.
- INR 5.0-9.0, minor bleeding (bruising, nosebleeds): Give 1-2.5 mg of oral vitamin K. Recheck INR in 24 hours.
- INR over 10, or major bleeding (vomiting blood, dark stools, headache, weakness): Give 5-10 mg IV vitamin K plus 4-factor prothrombin complex concentrate (PCC). Don’t wait. This is an emergency.
What Should You Do?
If you’re on warfarin:- Never start TMP-SMX without checking your INR first. Do it the same day.
- Check your INR again within 48-72 hours after starting the antibiotic.
- Ask your doctor: “Is there a safer antibiotic?” Say: “I’m on warfarin. Can we use nitrofurantoin or doxycycline instead?”
- Watch for signs of bleeding: Unusual bruising, pink or red urine, black stools, severe headaches, dizziness.
- Don’t stop warfarin on your own. Even if you feel fine, your INR could be rising silently.
What About New Blood Thinners?
DOACs - like apixaban, rivaroxaban, dabigatran - don’t interact with TMP-SMX the same way. That’s why many doctors now switch patients to them. But here’s the catch: 2.6 million Americans still take warfarin in 2025. Why?- People with mechanical heart valves - DOACs aren’t approved for them
- Cost - warfarin costs $10 a month. DOACs cost $300+
- Some patients do better on warfarin - their INR is stable, they’ve been on it for 20 years
Real Stories From Real Patients
One Reddit user shared: “My 78-year-old dad had a mechanical aortic valve. INR was 2.6. Got Bactrim for a UTI. Three days later, he collapsed. INR was 8.2. He needed vitamin K and FFP. He’s fine now, but we almost lost him.” Another pharmacist wrote: “I’ve seen patients take Bactrim with no INR change. But I’ve also seen 20-year-olds with no risk factors spike to 7.0. It’s unpredictable. That’s why we check.” There’s no such thing as ‘safe’ for everyone. Only ‘monitored’.Bottom Line
TMP-SMX and warfarin is a deadly combo - not because it’s rare, but because it’s predictable. And yet, it’s still prescribed. If you’re on warfarin:- Ask for alternatives before accepting TMP-SMX
- Get your INR checked before and after starting any antibiotic
- Know the signs of bleeding - and act fast
- Don’t assume you’re safe just because you’ve taken it before




Been a pharmacist for 12 years and I still see this happen. Docs prescribe Bactrim like it’s Advil. I had a 72-year-old come in last week with a GI bleed after a UTI script. INR was 9.4. He didn’t even know Bactrim was an issue. We need better alerts in EHRs - this isn’t rocket science.
THIS. So many people don’t realize how dangerous this is. If you’re on warfarin, never accept Bactrim without asking for nitrofurantoin. Seriously. Your life isn’t worth gambling with. Print this out and hand it to your doctor. Knowledge is power - and it saves lives.
i had a frnd who took bactrim and her inr went to 8. she was fine tho lol. maybe its just luck?
Of course you’re going to have bleeding events. You’re giving someone a potent CYP2C9 inhibitor on top of a narrow-therapeutic-index anticoagulant. This isn’t a ‘risk’ - it’s a pharmacokinetic disaster waiting to happen. The fact that this is still prescribed shows how broken our medical education system is. Medical students should be drilled on this before they touch a stethoscope.
Let me tell you something they don’t want you to know. The FDA doesn’t actually ban these combos because Big Pharma owns the FDA. They make billions off warfarin and the ER visits it causes. Bactrim is cheap. DOACs? Expensive. So they let people bleed out so the stock prices stay high. You think nitrofurantoin isn’t being suppressed? It’s not on the formulary in 70% of hospitals. Why? Because no one’s making money off it. Wake up. This isn’t medicine - it’s a profit scheme.
I’ve seen patients get discharged with INRs over 10 and no follow-up. No one’s monitoring. No one cares. The system is rigged. And you’re just a number in their spreadsheet.
They’ll tell you ‘it’s rare’ - but it’s only rare because most people die before they get to Reddit. My cousin’s neighbor’s cousin died from this. They buried him before his wife could even get his INR results.
Don’t trust your doctor. Don’t trust the system. Check your INR every 3 days if you’re on antibiotics. Buy a home monitor. Live like your life depends on it - because it does.
And if you’re one of those ‘it’s just a UTI’ people? You’re one fall away from a brain hemorrhage. And then your family will be left wondering why no one warned them.
Ugh, I’m so tired of this. I had my mom on warfarin for 15 years. She got Bactrim once - just once - and ended up in the ICU. They didn’t even tell her it was risky. I had to Google it myself. I’m not even mad - I’m just disappointed. We’re living in 2025 and doctors still treat patients like they’re dumb? It’s not just about the drug interaction - it’s about the arrogance. ‘Trust me, I’m a doctor.’ No. I trust data. And the data says: avoid TMP-SMX like the plague. Nitrofurantoin is safe. Use it. Demand it. Don’t let your doctor’s laziness kill you.
Also, men are 9% more at risk? That’s not a coincidence. It’s systemic. Women are more likely to question meds. Men just take what’s handed to them. That’s why my dad’s still alive and your uncle isn’t.
Really appreciate this breakdown. I’ve been on warfarin since 2018 after a DVT. I always ask for alternatives now - nitrofurantoin or doxycycline. My PCP thinks I’m overcautious, but I’d rather be safe than sorry. One time I got a script for Bactrim for a sinus infection - I called the pharmacy first and they flagged it. They called my doctor and switched it. That’s the kind of system we need more of.
Also, the vitamin K point is huge. I started eating more kale and broccoli. Not because I’m trying to ‘counteract’ warfarin - but because I’m trying to be healthier overall. Small changes matter.
Thank you for writing this. I’m a nurse in London and I’ve seen this exact scenario play out three times this year. One guy was on his 3rd hospital admission because he kept getting UTIs and getting Bactrim. He didn’t know it was the cause. We finally sat him down, showed him the INR trends, and switched him to nitro. He cried. Said he thought he was just ‘bad at staying healthy.’ We need more patient education - not just more meds.
Also, the PCC vs FFP point? Huge. FFP takes forever, floods the system, and risks volume overload. PCC is the future. If your hospital doesn’t stock it, ask why.
This is why I hate medicine. It’s all anecdotes and no data. ‘INR went to 7.1’ - cool. What was his baseline? What was his renal function? What was his CYP2C9 genotype? Did he take his warfarin at the same time? Did he drink alcohol? Did he eat a salad? No. Just ‘Bactrim = bad.’ That’s not science. That’s fearmongering. You’re turning a complex pharmacokinetic interaction into a meme. Grow up.
Life is balance. Warfarin, Bactrim, vitamin K - all part of the dance. To fear is to not understand. To understand is to accept.
I’m from India and we see this a lot here too. Doctors here often don’t even know about the interaction. I had a cousin who got Bactrim for a UTI and ended up in the ER. His INR was 7.8. He survived, but his family was terrified. We need more global awareness - this isn’t just a US problem. Warfarin users everywhere need to know.
Also, I’ve seen patients in rural clinics get Bactrim because it’s the only antibiotic in stock. No alternatives. No labs. No monitoring. It’s heartbreaking.
It is both a moral imperative and a clinical necessity to recognize the gravity of this pharmacological interaction. The confluence of CYP2C9 inhibition, protein displacement, and gut microbiome disruption constitutes a triad of iatrogenic peril that is not merely statistically significant - it is ethically indefensible that such a predictable cascade remains unmitigated in contemporary practice. The persistence of this prescribing pattern reflects a systemic failure of medical education, regulatory oversight, and patient advocacy. To prescribe trimethoprim-sulfamethoxazole to a patient on warfarin without contemporaneous INR monitoring is not negligence - it is negligence with premeditation. One must ask: if this were a new drug, would it ever have received FDA approval? The answer is self-evident. The fact that it persists is a testament not to efficacy, but to institutional inertia. We owe our patients better.