When you pick up a prescription at the pharmacy, you might not realize the pharmacist is making a legal decision that could save you hundreds of dollars-or even keep you safe. In most states, pharmacists can swap your brand-name drug for a cheaper generic version without asking your doctor. That’s called generic substitution. But what if they want to switch you to a different drug entirely-say, one from the same class but with a different chemical structure? That’s therapeutic substitution, and the rules around it vary wildly from state to state.
What Pharmacists Can and Can’t Do
Every state allows pharmacists to substitute generic drugs for brand-name ones. It’s not optional-it’s standard. The FDA requires generics to be bioequivalent, meaning they deliver the same amount of active ingredient into your bloodstream within a tight range (80% to 125% of the brand). This isn’t guesswork. Pharmacists check the FDA’s Orange Book, which lists over 13,700 approved therapeutic equivalents as of early 2024. If a generic is listed there, they can swap it.
But therapeutic substitution? That’s where things get messy. Therapeutic substitution means replacing a drug with another in the same class-like switching from one statin to another, or one antidepressant to a different one. Only 27 states explicitly allow this. In 23 states, pharmacists can’t do it at all unless the doctor gives written permission. Even in states that allow it, the rules differ. In Colorado, pharmacists must write “Intentional Therapeutic Drug Class Substitution” on the prescription. In California, they can only do it for insulin. In Maryland, they can now prescribe birth control directly. In Alabama? Not unless the doctor says so.
The Federal Twist: Paxlovid and Beyond
In July 2022, something unusual happened. The FDA gave pharmacists nationwide the authority to prescribe Paxlovid, an antiviral for high-risk COVID-19 patients. This wasn’t just substitution-it was prescribing. Pharmacists had to check age, weight, test results, and kidney or liver function. They had to confirm eligibility through electronic records or direct contact with the prescriber. This was the first time the federal government stepped in to expand pharmacy practice beyond substitution into direct prescribing. It set a precedent. If pharmacists can prescribe a high-risk antiviral, why not other medications?
Since then, states have followed suit. Maryland’s 2023 law lets pharmacists prescribe birth control with Medicaid coverage. New Mexico and Oregon let pharmacists manage chronic conditions like hypertension and diabetes under standardized protocols. These aren’t small changes-they’re shifts in how care is delivered. In rural areas, where doctors are scarce, pharmacists are becoming the first point of contact for medication management.

State-by-State Reality Check
There’s no national standard. A patient in Colorado can walk into a pharmacy and get birth control, a flu shot, and a switch to a cheaper blood pressure med-all in one visit. A patient in Texas might need to call their doctor just to swap one insulin for another. In Oklahoma, pharmacists can substitute insulin with documentation only. In Texas, they have to call the prescriber. That’s 15 to 20 extra minutes per prescription during busy hours.
Here’s how it breaks down:
- 49 states require pharmacists to notify patients when substituting generics.
- 17 states require written patient consent for therapeutic substitution.
- 14 states have no consent requirement at all-just documentation.
- 32 states require the substitution to be noted directly on the prescription.
- 14 states give pharmacists 72 hours to report the change.
- 19 states demand the prescriber be notified within 24 to 48 hours.
And it’s not just about paperwork. Electronic health records often don’t talk to each other. A pharmacist in Georgia might not know a patient’s substitution history from Alabama. Chain pharmacies like Kroger have cut substitution errors by 37% by creating their own cross-state protocols. But independent pharmacies? They’re left to figure it out alone.
Why It Matters: Cost, Access, and Safety
Generic substitution saves the U.S. healthcare system about $197 billion a year. Over the last decade, that’s $1.97 trillion. Therapeutic substitution adds more. The National Pharmaceutical Association estimates it could save another $45 to $60 billion annually if expanded. But it’s not just about money.
Over 60 million Americans live in areas with too few primary care doctors. In rural communities, pharmacist-led therapeutic substitution has cut medication access gaps by 34%. One pharmacist in Colorado told me she served 47 patients who couldn’t get a doctor’s appointment within 30 days-each visit took five minutes using a standardized form.
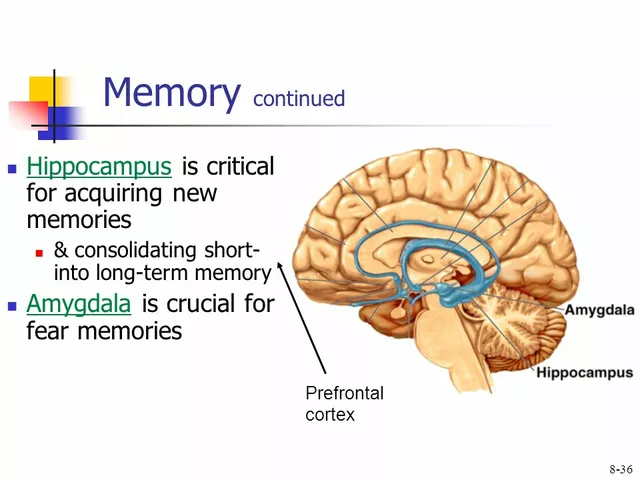
But there’s risk. Dr. David Fleming from the American College of Physicians warns that without access to full medical records, pharmacists might miss drug interactions or overlapping conditions. A patient on five meds for diabetes, heart failure, and depression? Switching one drug without seeing the full picture could backfire. That’s why experts like Dr. Lucinda Maine from the American Association of Colleges of Pharmacy support expansion-but only with better data sharing and standardized training.
Training, Tech, and the Road Ahead
Pharmacists in states with expanded authority need 10 to 15 extra hours of training. In Colorado, it’s 12.75 hours on protocols, documentation, and therapeutic equivalence. Pharmacists who work across state lines often need 40+ additional hours just to stay compliant. That’s time and money-something many small pharmacies can’t afford.
Technology is catching up. Some pharmacies now use automated alerts in their systems that flag when a substitution might conflict with a patient’s history. Insurance companies are slowly aligning reimbursement policies. But 52% of pharmacists still report issues getting paid for therapeutic substitutions because insurers don’t recognize them as billable services.
As of March 2024, 19 states are pushing new laws to expand pharmacist authority. Seven-Virginia, Illinois, and others-are expected to pass reforms by the end of the year. The American Pharmacists Association is pushing for national competency standards, so a pharmacist in Florida can practice the same way as one in Washington. But the American Medical Association still pushes back, arguing that doctors should remain in control.
What This Means for You
If you’re on a chronic medication and your pharmacist switches it, ask why. Did they pick a cheaper generic? Or did they swap in a different drug entirely? You have the right to know. In 12 states, they need your signature. In others, they just need to tell you. If you’re unsure, ask for the name of the original drug and the new one. Check the label. Look up the difference.
And if you live in a state with restrictive laws? Your pharmacist might be frustrated. They see you struggling with cost or access. They know a better option exists. But they’re legally blocked from helping. That’s not a failure of the pharmacist-it’s a failure of the system.
The future of pharmacy isn’t just filling prescriptions. It’s managing care. And the legal scope of practice is changing-slowly, unevenly, but undeniably.
Can my pharmacist switch my brand-name drug to a generic without asking me?
Yes, in all 50 states and D.C., pharmacists can substitute a generic version of your brand-name drug without contacting your doctor. But they must inform you-either verbally or in writing-before dispensing it. Some states require you to sign a form acknowledging the switch. Always check the label to confirm the drug name and manufacturer.
Can my pharmacist switch me to a different drug entirely, like a different antidepressant?
Only in 27 states, and even then, only under strict rules. Some states require patient consent, others require documentation, and a few only allow it for specific drugs like insulin. In most states, your pharmacist must call your doctor for permission. If you’re unsure, ask if the switch is a generic substitution or a therapeutic substitution-they’re not the same thing.
Why does my pharmacist in Colorado have more freedom than the one in Alabama?
Each state sets its own pharmacy laws. Colorado passed statewide protocols that let pharmacists prescribe birth control, manage chronic conditions, and perform therapeutic substitutions without individual doctor approval. Alabama still requires prescriber authorization for nearly every change. These differences exist because pharmacy practice is regulated at the state level, not federal. There’s no national standard, so your rights depend on where you live.
What’s the difference between generic and therapeutic substitution?
Generic substitution means swapping your brand-name drug for a chemically identical generic version-same active ingredient, same dose, same effect. Therapeutic substitution means replacing your drug with a different one from the same class-like switching from lisinopril to losartan, both blood pressure meds, but with different chemical structures. Generic substitution is legal everywhere. Therapeutic substitution is legal only in 27 states and comes with heavy restrictions.
Can pharmacists prescribe medications now?
Yes, but only in specific cases and only in certain states. Since July 2022, pharmacists nationwide can prescribe Paxlovid for eligible COVID-19 patients. In Maryland, they can prescribe birth control. In New Mexico and Oregon, they can manage chronic conditions like hypertension under state-approved protocols. These are not blanket prescribing rights-they’re limited, condition-specific authorities granted by state law or federal emergency authorization.




Had my blood pressure med switched last month and didn’t even notice until I checked the bottle. Saved me $80 a month. Pharmacists are unsung heroes.
Always ask if it’s generic or therapeutic-big difference.
Oh great. So now we’re letting chemists play doctor because ‘cost savings’? Let’s not forget the last time we outsourced medical judgment to people who don’t even have an MD after their name. You think a pharmacist reading a label knows what happens when you mix a new statin with your anticoagulant? No. They just see ‘bioequivalent’ and cash in. This isn’t progress-it’s corporate negligence dressed up as ‘innovation.’
Let’s be clear: therapeutic substitution isn’t about convenience-it’s about system optimization under resource constraints. Pharmacists, as medication therapy management (MTM) providers, are uniquely positioned to reduce polypharmacy risks when integrated into care teams with standardized protocols and EHR interoperability.
States that restrict this are artificially bottlenecking care delivery, especially in HPSA zones. The AMA’s resistance is rooted in turf protection, not patient safety. Evidence from Colorado and Oregon shows improved adherence and reduced ED visits. We need national competency benchmarks, not state-by-state chaos.
Y’all act like pharmacists are gonna start handing out insulin like candy. LOL. We got folks in Texas tryna swap your heart med for some cheap-ass generic because the insurance company told ‘em to. Meanwhile, your grandma’s kidneys are failin’ and no one’s checkin’ her labs. This ain’t ‘progress,’ it’s a $$$-driven free-for-all. And don’t even get me started on how the big chains track your med history across states-good luck if you’re in a mom-and-pop shop with a fax machine and a prayer.
Interesting how the U.S. treats pharmacy like a patchwork quilt-each state stitching its own rules. In South Africa, pharmacists have had expanded roles for years, especially in rural clinics where doctors are rare. They manage HIV meds, diabetes, even mental health follow-ups under clear guidelines. The difference? We trust the profession, and we train them rigorously.
Here, it’s all politics. If you’re in Colorado, you get birth control from your pharmacist. In Alabama? You wait six weeks for a doctor who might not even take your insurance. This isn’t healthcare-it’s geography-based luck.
Wait… so now pharmacists can prescribe Paxlovid but you can’t trust them to switch your antidepressant? That’s not logic, that’s a secret government agenda. The FDA doesn’t just ‘allow’ this out of the goodness of their heart. They’re testing control mechanisms. Next thing you know, your meds will be auto-changed via AI and your doctor won’t even know. Big Pharma’s been pushing this for years to kill off the need for specialists. You think your pill bottle is safe? Think again.
People act like this is about saving money. But what about the moral responsibility? You don’t swap a person’s mental health meds like a coupon. That’s not healthcare-that’s commodification. And now we’re letting people who didn’t go to med school make decisions that could alter someone’s life? Where’s the accountability? If I mess up my taxes, I get fined. If a pharmacist messes up my meds, someone could die. And no one’s holding them accountable.
Generic substitution is a well-documented, FDA-regulated process with strict bioequivalence thresholds (80–125% AUC/Cmax). Therapeutic substitution, however, introduces pharmacodynamic variability-different receptor affinities, half-lives, and metabolite profiles. Even within the same class, switching from sertraline to fluoxetine can alter CYP450 interactions, especially in polypharmacy patients.
Current state protocols lack uniformity in clinical decision support integration. Until EHRs can dynamically flag drug-class interactions across state lines, therapeutic substitution remains a high-risk, low-reward proposition. Mandatory training modules and real-time pharmacy alerts are non-negotiable prerequisites for expansion.
bro i live in india and here pharmacists can’t even give you insulin without a scrip… but i’ve seen them give advice on meds like they’re doctors. maybe us non-us folks just don’t get how much freedom y’all have. but also… how do u even know if ur med was switched? labels look the same. i’d be scared to even ask.
While I appreciate the intent behind expanding pharmacist roles, the legal and ethical framework remains underdeveloped. The absence of mandatory prescriber notification windows, inconsistent documentation standards, and lack of interoperable data systems create significant liability risks. This is not a matter of professional autonomy-it is a matter of systemic fragility. Until the infrastructure catches up, incremental reform is not merely prudent-it is imperative.
Let’s not romanticize this. Pharmacists are trained to dispense, not diagnose. But in places where doctors are 100 miles away, they become the only line of defense. I’ve seen it in rural South Africa-pharmacists managing HIV regimens, checking blood pressure, adjusting doses based on lab results they get from clinics once a month. It’s messy. It’s imperfect. But it saves lives.
So yes, expand their scope-but pair it with funding, training, and real-time data access. Don’t just hand them more power and walk away. That’s not innovation. That’s abandonment with a badge.