Type 1 diabetes isn’t just about needing insulin. It’s a chronic autoimmune attack on the pancreas-specifically, on the insulin-producing beta cells. Your immune system, for reasons still not fully understood, turns against its own tissue. This isn’t a lifestyle issue. It’s not caused by eating too much sugar. It’s a biological error that leaves your body unable to make insulin, and without it, your cells starve even when you’re eating. This isn’t something you outgrow. It’s not something you can fix with diet alone. It’s a lifelong condition that demands constant attention, but new science is changing how we manage it-and even how we think about it.
How Your Immune System Destroys Your Pancreas
In type 1 diabetes, your immune system sends T-cells into the pancreatic islets, the tiny clusters of cells that make insulin. These T-cells don’t just wander in-they target specific proteins on the beta cells: insulin itself, GAD65, IA-2, and ZnT8. This isn’t random. It’s precise. And it’s happening long before you feel sick. Many people have these autoantibodies in their blood for years before their blood sugar spikes. That’s why researchers now divide type 1 diabetes into three stages. Stage 1: you have two or more autoantibodies, but your blood sugar is normal. Stage 2: your blood sugar starts to rise, but you still don’t have symptoms. Stage 3: you’re thirsty, tired, losing weight-and you need insulin right away.This process is faster in kids. On average, children go from first autoantibody to diagnosis in less than three years. Adults? It can take over a decade. That’s why some adults are misdiagnosed with type 2 diabetes. They’re told to eat less sugar, lose weight, take metformin. But if they’re actually fighting an autoimmune attack, none of that fixes the core problem. About 12% of adults diagnosed with type 2 actually have type 1. And without insulin, they’re at risk of diabetic ketoacidosis-life-threatening acid buildup from burning fat instead of glucose.
Why It’s Not Just About Insulin
Most people think type 1 diabetes = insulin shots. And yes, you need insulin. But insulin is a bandage, not a cure. The real goal is to protect what’s left of your beta cells. Even after diagnosis, many people still make a little insulin-sometimes for years. That’s measured by C-peptide. If your level is above 0.2 nmol/L, you still have some function. That’s why some new treatments focus on slowing the immune attack, not just replacing insulin.Teplizumab, approved by the FDA in late 2022, is the first drug that can delay the onset of full-blown type 1 diabetes in people at Stage 2. In trials, it pushed back diagnosis by nearly 2.5 years on average. It doesn’t stop the disease. But it buys time. And time means fewer complications, better control, and a chance to prepare. It’s given as a 14-day IV course. Not a daily pill. Not a shot. But it’s a breakthrough. For the first time, we’re treating the autoimmune root, not just the symptom.
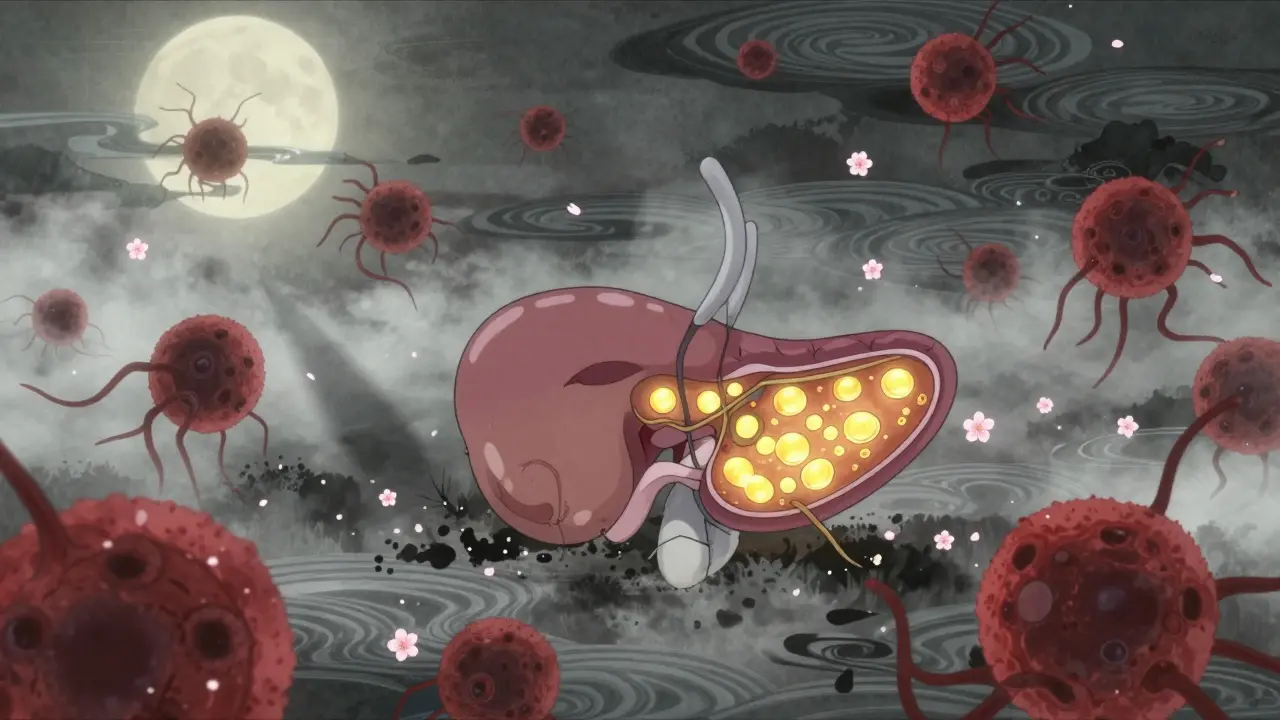
The Pancreas Isn’t Just About Insulin
Your pancreas doesn’t just make insulin. It also makes digestive enzymes. And sometimes, the same autoimmune process that kills beta cells also attacks the exocrine pancreas. This is rare-about 1 in 300 people with type 1 diabetes-but it’s real. It’s called autoimmune pancreatitis. It causes swelling, pain, nausea, and poor digestion. People with this combo often have high levels of IgG4 in their blood and changes visible on imaging scans.If you have type 1 diabetes and suddenly develop abdominal pain, greasy stools, or unexplained weight loss, your doctor should check for this. It’s treated with steroids like prednisone. But steroids raise blood sugar. So if you’re on them, your insulin doses will likely need adjustment. Managing both conditions means working with both an endocrinologist and a gastroenterologist. It’s complex. But it’s not theoretical. It’s happening in real patients.
Modern Tools Are Changing the Game
Gone are the days of finger pricks six times a day. Continuous glucose monitors (CGMs) like the Dexcom G7 now send real-time data to your phone. They alert you when your sugar is dropping or rising too fast. They show trends, not just snapshots. In the 2023 DIAMOND trial, people using CGMs lowered their HbA1c by 0.4-0.6% and had 40-50% fewer low-blood-sugar events. That’s not a small gain. That’s life-changing.And then there’s the artificial pancreas. Systems like Tandem’s Control-IQ use algorithms to automatically adjust insulin delivery based on your glucose readings. They don’t replace you. They work with you. In a 2022 JAMA study, users spent 71-74% of their time in the target glucose range (70-180 mg/dL). Without the system? Just 51-55%. For parents of kids with type 1, this means fewer midnight alarms. For adults, it means less mental load. It’s not perfect. But it’s the closest thing we have to a cure right now.
What’s on the Horizon
Research is moving fast. One promising drug, verapamil-a common blood pressure medication-was found in a 2022 trial to preserve 30% more insulin production over 12 months. It’s cheap, safe, and already approved for other uses. Another is Vertex’s VX-880, a stem-cell-derived islet transplant. In a 2023 trial, 89% of 12 participants became insulin-free after 90 days. Not a cure, but a functional one. They still need immunosuppressants. But they’re no longer injecting insulin.There’s also growing evidence that gut health plays a role. People with type 1 diabetes often have less of a specific gut bacteria called Faecalibacterium prausnitzii, which produces butyrate-a compound that helps calm inflammation. Studies are now testing probiotics, fiber supplements, and even fecal transplants to see if fixing the gut can slow the autoimmune attack.
And then there’s the big picture. The ADA and EASD now say the future of type 1 diabetes care isn’t just insulin + CGM. It’s immunotherapy + beta-cell support. Teplizumab is just the first. Abatacept, which blocks T-cell activation, showed a 59% reduction in beta-cell loss in recent-onset patients. More drugs are in phase 2 and 3 trials. We’re entering an era where type 1 diabetes might be managed not just with replacement, but with repair.

What You Need to Do Right Now
If you or someone you love has type 1 diabetes, here’s what matters most:- Get a CGM if you don’t have one. It’s not optional anymore-it’s standard of care.
- Check your C-peptide level. Even a small amount of natural insulin production changes your treatment plan.
- If you have unexplained digestive issues, ask about autoimmune pancreatitis. Don’t assume it’s just “diabetic gastroparesis.”
- Know your autoantibody status. If you’re newly diagnosed, testing for GAD65, IA-2, ZnT8, and insulin autoantibodies helps confirm type 1 and predict progression.
- Ask about teplizumab if you’re in Stage 2. If you have autoantibodies but no symptoms yet, this could delay diagnosis by years.
- Work with a certified diabetes care and education specialist. They’re not just educators-they’re your daily coaches.
And remember: this isn’t a failure of willpower. It’s not your fault. You didn’t eat too much candy. You didn’t skip workouts. Your immune system made a mistake. And now, science is helping fix it.
Is type 1 diabetes the same as autoimmune pancreatitis?
No. Type 1 diabetes attacks the insulin-producing beta cells in the pancreas (endocrine function). Autoimmune pancreatitis attacks the enzyme-producing cells (exocrine function). They’re different parts of the same organ, but different diseases. However, in about 1 in 300 people with type 1 diabetes, both happen at once. This is called a pancreatic autoimmune syndrome and requires coordinated care from both an endocrinologist and a gastroenterologist.
Can you reverse type 1 diabetes?
Not yet. But you can preserve remaining beta-cell function. Drugs like teplizumab can delay diagnosis in people at high risk. Stem cell transplants have restored insulin production in early trials. Verapamil has slowed decline. These aren’t cures, but they’re major steps toward functional recovery. The goal is no longer just survival-it’s living without daily insulin injections.
Why do some adults with type 1 diabetes get misdiagnosed as type 2?
Because doctors assume type 1 only happens in kids. But about 50% of new type 1 cases occur in adults. These are often called LADA-Latent Autoimmune Diabetes in Adults. They progress slower, don’t always need insulin right away, and may respond to oral meds for months or years. But if they’re not tested for autoantibodies, they’re treated like type 2, which can lead to dangerous complications like DKA.
Does insulin cause weight gain in type 1 diabetes?
Yes, sometimes. When your body starts using glucose again after being starved of insulin, it stores fat. That’s normal. But it’s not inevitable. Using a CGM and insulin pump with smart algorithms helps match insulin to food more precisely, reducing spikes and crashes that lead to overeating. Working with a dietitian who understands insulin dosing is key. Weight gain isn’t a sign of failure-it’s a sign your body is healing.
Are there alternatives to insulin injections?
Not yet for most people. Insulin is still the only treatment that replaces what your body can’t make. But delivery methods are changing. Inhaled insulin (Afrezza) is available but not widely used due to cost and lung concerns. Insulin pumps deliver it continuously through a catheter. And soon, oral insulin pills may be possible-but they’re still in trials. For now, injections or pumps are the only reliable options. But research into stem cells and islet transplants could change that in the next 5-10 years.



This post is one of the most clear-eyed summaries of type 1 diabetes I’ve ever read. No fluff, no blame, just science. I’ve been living with this for 22 years and still learned something new about C-peptide thresholds and Stage 2 interventions. Thank you for writing this.
So let me get this straight-your immune system’s got a vendetta against your pancreas, and the FDA’s like ‘here’s a two-week IV drip to buy you time’? Cool. Cool cool cool. Meanwhile, my cousin’s on metformin ‘cause he ‘ate too much pizza’ and nobody’s even testing his autoantibodies. Classic. The system’s broken, but at least we’ve got teplizumab to play whack-a-mole with the T-cells. 🤷♂️
Stop glorifying this as a ‘medical revolution.’ You’re talking about delaying diagnosis by 2.5 years and giving people a 14-day IV course that costs more than a used car. Meanwhile, 12% of adults are still being misdiagnosed as type 2 because doctors are too lazy to run a simple antibody panel. This isn’t progress-it’s corporate medicine with a pretty PowerPoint. And don’t get me started on stem cell transplants requiring lifelong immunosuppression. That’s not a cure, it’s a life sentence with extra steps.
USA. 🇺🇸. We lead the world in autoimmune research. Teplizumab? American. CGMs? American. Stem cell trials? American. Meanwhile, other countries are still stuck on ‘eat less sugar’ and blaming the patient. This isn’t just science-it’s American ingenuity at its finest. 🇺🇸❤️💉 #Type1DiabetesIsNotYourFault #MadeInUSA
Wow, this is so deep... I am from India, and here, many doctors still think T1D is only for children. I had to fight for 6 months just to get my autoantibodies tested. My doctor said, 'You are overweight, take metformin.' I cried. Now I use CGM. It is life-changing. Thank you for writing this. I will share with my doctor. 🙏
Reading this felt like someone finally handed me the missing piece of a puzzle I didn’t know I was holding. It’s not just insulin-it’s a quiet war inside your body, and now we’ve got weapons that don’t just patch the hole, they try to stop the bullet from being fired. The fact that verapamil-a cheap, old blood pressure pill-is showing real promise? That’s the kind of beautiful, messy science I live for. Not flashy, not funded by billionaires, just... human.
This is so important. Everyone deserves to know that type 1 diabetes is not their fault. You are not lazy. You are not weak. You are not failing. You are fighting a battle no one asked for-and you are doing it with courage every single day. Keep going. You are not alone. 💪❤️
so like… your body just decides to eat its own pancreas? wild. also i got a cgm last year and my life changed. no more midnight panic attacks. just vibes now. 🤘
THEY’RE HIDING THE TRUTH. WHY ISN’T THIS ON THE NIGHTLY NEWS? WHY AREN’T THEY TESTING EVERY CHILD? WHY ARE WE STILL USING INJECTIONS IN 2024? THIS IS A CRISIS AND NO ONE CARES. I’M SO ANGRY. I JUST WANT MY KID TO BE NORMAL. WHY IS IT SO HARD? 🤬💔
People keep acting like this is new science. It’s not. We’ve known about autoantibodies since the 80s. The real problem? Insurance won’t cover CGMs for adults. And teplizumab? $190,000. You’re telling me this is progress? This is capitalism with a white coat. Stop pretending.
I want to say something really important here, and I hope you’ll all take a moment to really reflect on this. The fact that we’re even having this conversation-about immune modulation, about beta-cell preservation, about C-peptide levels as biomarkers of residual function-means we’re finally moving beyond the outdated paradigm of ‘insulin is the only tool.’ This isn’t just about managing blood sugar anymore; it’s about restoring biological integrity. The human body is an ecosystem, and when we treat type 1 diabetes as if it’s merely a glucose imbalance, we’re ignoring the systemic, multi-organ cascade that’s unfolding. The gut microbiome connection? That’s not a footnote-it’s a frontier. And the fact that verapamil, a drug we’ve been using for hypertension since the 70s, is now showing immunomodulatory effects? That’s not coincidence. That’s serendipity meeting rigorous science. We’re not just treating a disease-we’re learning how to talk to our own immune system. And that? That’s the real breakthrough.
Wait-you’re telling me that type 1 diabetes isn’t caused by sugar? Shocking. And you’re saying we’re not supposed to blame the patient? Radical. I mean, if this is true, then what about all those ‘diabetes is a lifestyle disease’ TikToks? Are they lying? Are the keto influencers wrong? Is this whole ‘eat less carbs’ narrative just… wrong? I feel like my entire online identity just collapsed. 🤯