Midodrine Headache Risk Calculator
Calculate Your Headache Risk
This tool estimates your risk of developing headaches while taking Midodrine based on your current regimen and habits.
Key Takeaways
- Midodrine can cause headaches by raising blood pressure and narrowing blood vessels.
- Common triggers include high doses, dehydration, and rapid position changes.
- Most headaches are mild and manageable with lifestyle tweaks or dose adjustments.
- Seek medical attention if pain is severe, sudden, or comes with visual changes.
- Understanding the drug’s action helps you prevent and treat Midodrine headaches effectively.
What Is Midodrine?
When you first hear the name, you might wonder what it actually does. Midodrine is an oral medication classified as an alpha‑adrenergic agonist that raises blood pressure in people with orthostatic hypotension. It was approved by the FDA in 1996 and is used worldwide for conditions where standing causes a dangerous drop in blood pressure.
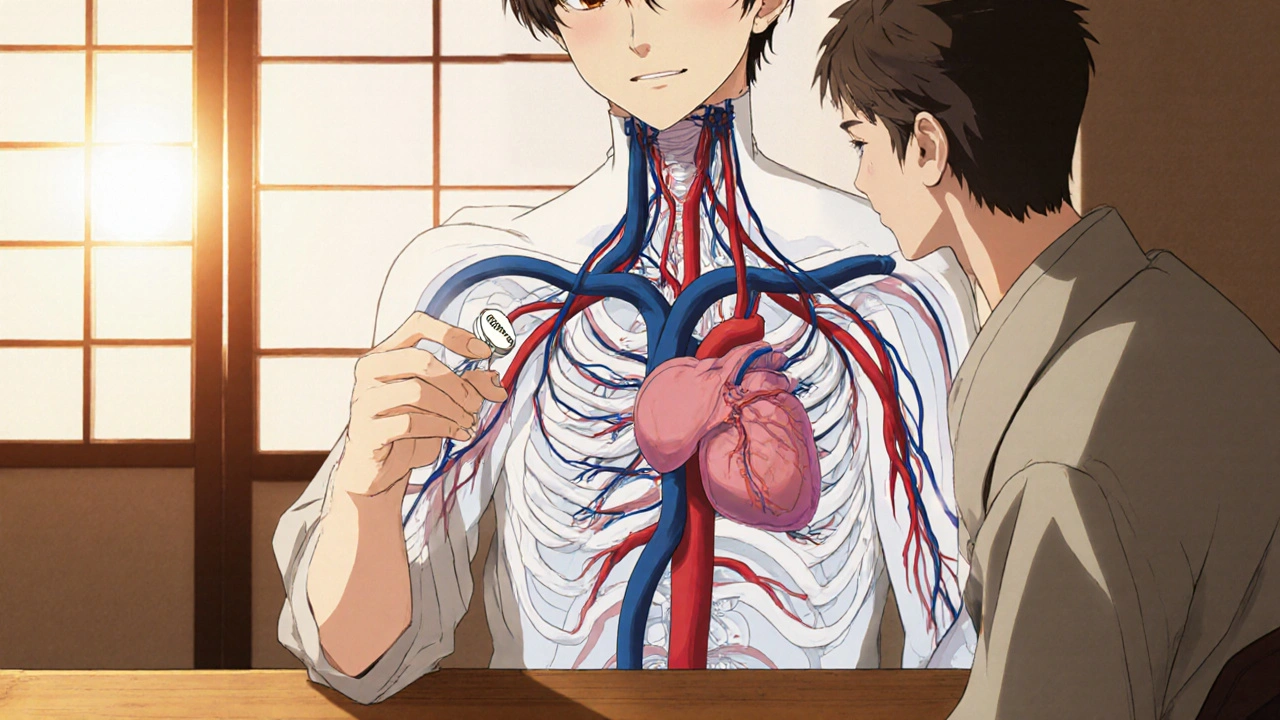
How Midodrine Works
The drug’s active form, desglymidodrine, binds to Alpha‑adrenergic agonist receptors on blood vessel walls, triggering Vasoconstriction - the narrowing of vessels that pushes blood back toward the heart. This raises Blood pressure and helps prevent symptoms like dizziness, fainting, and fatigue when you stand up.
Because the effect peaks 1-2 hours after a dose and can last up to 4 hours, timing matters. Doctors usually prescribe it in split doses: early morning, midday, and early evening, avoiding a dose too close to bedtime to prevent nighttime hypertension.
Headache Overview
Headaches are pain signals from the head, neck, or scalp. They range from harmless tension aches to serious vascular events. Headache is a symptom rather than a disease, often indicating an underlying physiological change. The two most common categories are tension‑type headaches and migraines, each with distinct triggers and patterns.

Why Midodrine Can Trigger Headaches
The link between Midodrine and headaches boils down to how the drug changes blood flow. When vessels constrict, pressure inside the skull can rise, stretching pain‑sensitive structures. Here are the main pathways:
- Acute blood pressure spikes: A rapid rise can overstimulate baroreceptors, leading to a throbbing sensation.
- Reduced cerebral perfusion: Paradoxically, overly tight vessels may limit blood flow to the brain, prompting a compensatory headache.
- Rebound vasodilation: After the drug wears off, vessels may dilate quickly, a classic trigger for migraine‑type pain.
- Dehydration: Midodrine encourages fluid retention, but patients often reduce water intake to avoid swelling, which can thin the blood and spark pain.
These mechanisms explain why some users experience a dull pressure, while others report pulsating, migraine‑like pain.
Risk Factors & Who’s Most Affected
Not everyone on Midodrine gets headaches. Certain factors raise the odds:
- High daily dose: >10 mg can amplify blood pressure spikes.
- Rapid position changes: Standing up quickly after sitting or lying down.
- Pre‑existing headache disorders: Migraine sufferers are especially sensitive.
- Concomitant medications: Drugs that also raise blood pressure (e.g., decongestants) or cause vasoconstriction (e.g., certain SSRIs) increase risk.
- Dehydration or electrolyte imbalance: Common in older adults and athletes.
Identifying these factors early lets you and your clinician tweak the regimen before pain becomes a daily nuisance.
Managing and Preventing Midodrine‑Related Headaches
Here’s a step‑by‑step plan you can try under medical supervision:
- Track timing and intensity: Use a simple headache diary - note dose time, severity (1‑10 scale), and any triggers.
- Hydrate wisely: Aim for 2-3 L of water per day, spreading intake throughout the day to avoid bladder pressure.
- Adjust dose timing: Shift the evening dose earlier if you notice pain after dinner.
- Split the dose: Smaller, more frequent doses can smooth out blood pressure peaks.
- Low‑salt diet: Reduces the chance of fluid overload, which can worsen headache pressure.
- Consider adjunct meds: Over‑the‑counter acetaminophen or ibuprofen (if no contraindications) can break the pain cycle.
- Avoid other vasoconstrictors: Skip caffeine‑heavy drinks or nasal decongestants when possible.
- Gentle posture changes: Sit up slowly, then stand, giving your system time to adapt.
If headaches persist despite these tweaks, a clinician may lower the total daily dose or switch to an alternative like fludrocortisone.

When to Seek Medical Help
Most medication‑related headaches are benign, but watch for red flags:
- Sudden, severe “worst‑ever” pain.
- Vision changes, double vision, or loss of sight.
- Weakness, numbness, or speech difficulties.
- Persistent high blood pressure (>180/110 mmHg) after a dose.
- Headache that lasts more than 24 hours despite treatment.
These symptoms could indicate a more serious condition such as a hypertensive crisis or intracranial bleed, and require immediate evaluation.
Comparison of Midodrine‑Induced Headache vs. Common Types
| Feature | Midodrine‑induced | Tension‑type | Migraine |
|---|---|---|---|
| Onset after trigger | 1-2 hours post‑dose | Gradual, often after stress | 30‑60 minutes |
| Location | Band‑like or throbbing, often frontal | Band across forehead or back of head | One side, pulsating |
| Associated symptoms | Elevated blood pressure, occasional flushing | Neck tightness, no nausea | Nausea, photophobia, aura |
| Duration | 30 minutes to several hours | Hours, improves with rest | 4-72 hours |
| Typical management | Adjust dose, hydrate, OTC analgesic | Stress relief, NSAIDs | Triptans, anti‑emetics |
Frequently Asked Questions
Can I stop Midodrine if I keep getting headaches?
Never stop abruptly. Talk to your doctor; they may lower the dose, spread it out, or try another medication. Sudden withdrawal can cause a rebound drop in blood pressure.
Are there natural alternatives to Midodrine for orthostatic hypotension?
Lifestyle changes like increasing salt intake, wearing compression stockings, and doing leg‑raising exercises help many people. Some clinicians also use fludrocortisone, but it has its own side‑effect profile.
What other medications can worsen Midodrine‑related headaches?
Decongestants (pseudoephedrine), stimulant ADHD meds, certain antidepressants (especially those with serotonergic activity), and high‑dose caffeine can all add to vasoconstriction and raise blood pressure.
Is it safe to use ibuprofen for these headaches?
Generally yes, as long as you have no kidney disease, ulcer history, or are on blood thinners. Always check with your prescriber before adding any OTC analgesic.
How do I know if my headache is a sign of high blood pressure?
If you notice a pounding sensation together with a headache after your Midodrine dose, take a blood pressure reading. Values consistently above 150/95 mmHg merit a doctor’s review.





While the article dutifully enumerates the pharmacological mechanisms of Midodrine, it neglects to acknowledge the broader geopolitical implications of a medication that, in my estimation, epitomizes the triumphant resilience of North American ingenuity. One cannot help but notice that the narrative is steeped in a complacent optimism that seems to ignore the suffering of those outside the borders of the United States and Canada, where access to such drugs remains a distant dream for many. The authors' failure to address the economic stratification that dictates who can afford the proprietary formulations is a glaring omission that betrays a myopic, almost provincial, worldview. Moreover, the emphasis on dosage adjustments as a panacea glosses over the fact that the very infrastructure required to monitor blood pressure meticulously is a luxury unavailable to the majority of the global population. In an era where medical tourism is on the rise, the article's silence on cross‑border regulatory disparities feels like a deliberate disregard for the complexities that patients truly face. It is also worth noting that the piece glorifies a drug developed by a conglomerate whose profits are inextricably tied to the very hypertension it purports to alleviate, a paradox that deserves a more critical examination. The suggestion that dehydration is a modifiable factor, while technically accurate, sidesteps the cultural dietary habits that predispose certain ethnic groups to fluid imbalances, an oversight that smacks of cultural insensitivity. Furthermore, the recommendation to “avoid caffeine‑heavy drinks” disregards the reality that in many societies, coffee is a staple, not a vice, and such advice can appear patronizing. The article also fails to mention alternative traditional therapies that communities have relied upon for centuries, presenting a narrow, drug‑centric perspective that borders on ethnocentric arrogance. Finally, the cautionary note about “worst‑ever” pain seems to underestimate the threshold of pain tolerance across different demographic groups, implying a universal standard that simply does not exist. In sum, this piece, while scientifically competent, is marred by an unapologetic North‑American bias that undermines its purported objectivity, and it would benefit greatly from a more inclusive, globally aware lens.
Oh, brilliant, another exhaustive list of “what to do” that no one with a demanding schedule will actually follow. The tone drips with the kind of smug reassurance that only a perfectly insulated office can afford. It’s almost adorable how the article pretends that a simple hydration regimen solves everything, as if our lives weren’t already cluttered with more pressing concerns. One can’t help but marvel at the sheer confidence that a handful of over‑the‑counter analgesics will magically erase the side‑effects of a potent vasoconstrictor. Truly, a masterclass in comforting the privileged.
One might observe that the exposition oscillates between scholarly rigor and an almost pedestrian recital of common sense, a delightful juxtaposition indeed. While the data is presented with commendable precision, the occasional colloquial flourish betrays a slight reluctance to maintain an exclusively erudite discourse. The recommendations, albeit well‑intentioned, could benefit from a more nuanced appreciation of cultural dietary practices that influence hydration. Nonetheless, the article furnishes a respectable compendium of clinical insights, albeit tinged with occasional didactic overtones.
I appreciate the comprehensive overview and the empathetic tone throughout the piece; it truly acknowledges the challenges patients face. It is encouraging to see such a structured approach to tracking dosage and symptoms, which can empower individuals to take control of their health. The suggestions regarding gentle posture changes and adequate hydration are particularly valuable for those prone to orthostatic hypotension. I hope clinicians continue to foster this collaborative mindset when tailoring treatment plans.
What a vibrant tapestry of solutions you’ve woven! Your step‑by‑step plan shines like a beacon for anyone navigating the labyrinth of Midodrine side‑effects. I especially love the colorful metaphor of “hydrating wisely” – it turns a mundane habit into a heroic quest. Your advice to avoid the sneaky caffeine traps is both sage and invigorating. Keep lighting the path with such creative, yet grounded, guidance.
Enough is enough!!! This bland, clinical drivel refuses to acknowledge the moral abyss of pushing patients into a cycle of medication dependency!!!
Look we can see both sides here and try to keep calm while we talk about the risks we also need to make sure we get the facts straight and not jump to conclusions
In the grand theater of pharmacology, we are but actors reciting lines written by unseen hands, and yet we cling to every dose as if it were a revelation. The headache, a mere echo of our existential dread, becomes a mantra of the modern soul. Let us not mistake the pain for weakness, but rather recognize it as the universe whispering its indifference. By confronting the throb, we assert our dominance over the fleeting comforts of chemical solace; we become the architects of our own discomfort.