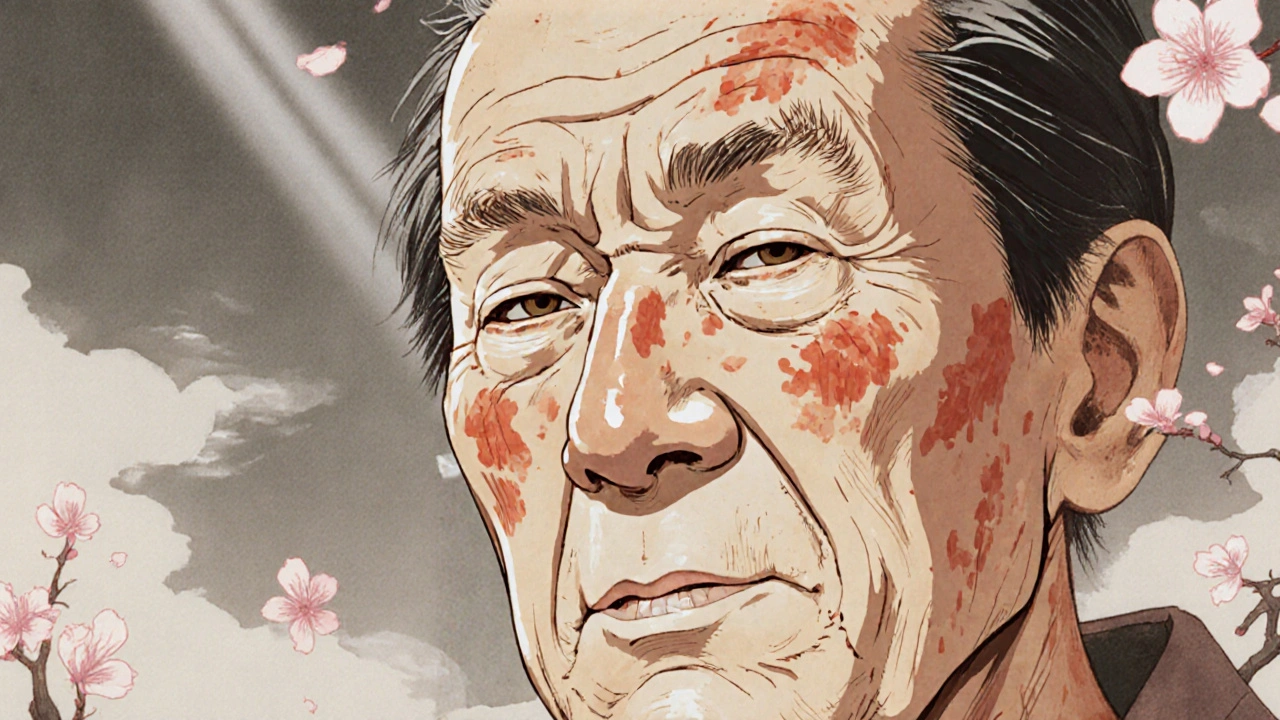
Spot a rough, scaly patch on your nose, cheeks, or scalp that won’t go away? It might not be just dry skin. If you’ve spent years in the sun-especially in places like Adelaide where UV levels stay high even in winter-you could be dealing with actinic keratosis. This isn’t a cosmetic issue. It’s your skin’s warning sign that sun damage has gone deep enough to change how cells grow. And it’s more common than most people realize.
What Exactly Is Actinic Keratosis?
Actinic keratosis (AK), also called solar keratosis, is a precancerous skin growth caused by long-term exposure to ultraviolet (UV) light. It starts as a tiny, rough spot-like sandpaper under your fingers. Over time, it can grow larger, turn red or brown, and sometimes itch or sting. These patches usually show up on sun-exposed areas: face, ears, scalp (especially if you’re bald), neck, forearms, and the backs of hands.
Think of it as a cellular glitch. UV radiation damages the DNA in your skin’s outer layer (the epidermis). The body tries to fix it, but repeated damage overwhelms the repair system. Cells start multiplying abnormally. About 10% of untreated actinic keratoses can turn into squamous cell carcinoma, a type of skin cancer. That’s why early detection matters.
How Skin Pigmentation Changes with Actinic Keratosis
One of the trickiest parts about AK is how it plays with skin color. It doesn’t always look the same. In lighter skin tones, you’ll often see red or pink patches. But in people with darker skin, those same lesions can appear as dark brown or black spots-sometimes mistaken for moles or age spots.
This variation happens because melanin, the pigment that gives skin its color, reacts differently to UV damage depending on your genetics. Darker skin has more melanin, which can mask the redness of early lesions. But the underlying cell damage is still there. That’s why people with darker skin often get diagnosed later-and why AK can be overlooked in non-white patients.
A study from the Journal of the American Academy of Dermatology found that nearly 30% of AK cases in people with Fitzpatrick skin types IV-VI were misdiagnosed as seborrheic keratosis or melasma. The result? Delayed treatment and higher risk of progression.
Who’s Most at Risk?
You don’t have to be an outdoor athlete or lifeguard to get AK. Risk factors include:
- Age over 40-cumulative sun exposure adds up over decades
- Light skin, blue eyes, or red or blonde hair-less natural UV protection
- Living in sunny climates like Australia, where UV levels are among the highest in the world
- History of sunburns, especially in childhood
- Weakened immune system-from medications, illness, or organ transplants
- Using tanning beds-even once increases your risk
In Australia, one in three adults over 40 has at least one actinic keratosis. In South Australia, rates are even higher due to intense summer UV and outdoor lifestyles. The good news? Most cases are caught early because they’re visible. The bad news? Many people ignore them, thinking they’re just "sun spots."

How to Spot the Difference Between AK and Normal Skin Changes
Not every rough patch is AK. Here’s how to tell:
- Actinic keratosis: Feels gritty or scaly, often smaller than a pencil eraser, may be tender or sting when touched, doesn’t go away after a few weeks, color can vary from flesh-toned to reddish or dark brown
- Seborrheic keratosis: Waxy, stuck-on appearance, usually brown or black, doesn’t feel rough, common in older adults, not caused by sun damage
- Moles: Smooth, round, even borders, usually symmetrical, color is consistent
- Age spots (liver spots): Flat, uniformly brown, no texture, harmless
If you’re unsure, don’t guess. Use the "ABCDE" rule adapted for AK: Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, Evolving over time. If it’s changing, growing, or bleeding-see a dermatologist.
What Happens If You Ignore It?
Some people wait because AK doesn’t hurt. Others think it’ll go away on its own. It won’t. Left untreated, about 1 in 10 AKs will become squamous cell carcinoma. That doesn’t mean it will spread to other organs-most are caught before that-but untreated skin cancer can grow deeper, damage tissue, and require surgery that leaves scars or disfigurement.
There’s also a phenomenon called "field cancerization." That means if you have one AK, your entire sun-damaged area-your face, scalp, or arms-is at higher risk for more lesions. Treating just one spot isn’t enough. You need to treat the whole field.

How It’s Diagnosed and Treated
A dermatologist can usually spot AK just by looking. But if it’s thick, bleeding, or unusual, they might take a small biopsy to rule out cancer.
Treatment options depend on how many lesions you have, where they are, and your skin type:
- Cryotherapy: Freezing with liquid nitrogen. Fast, cheap, and common. The spot blisters and peels off in 1-2 weeks.
- Topical creams: Fluorouracil (5-FU) or imiquimod. Applied daily for weeks. Can cause redness, peeling, and irritation-but clears large areas.
- Photodynamic therapy (PDT): A light-sensitive solution is applied, then activated with a special light. Great for large areas like the scalp or face.
- Chemical peels or laser therapy: Used for stubborn or cosmetically sensitive areas.
There’s no one-size-fits-all. A 70-year-old with 20 lesions on their scalp might need PDT. Someone with one small patch on their cheek might do fine with cryotherapy. Your doctor will pick the best option based on your skin and lifestyle.
Prevention Is the Best Medicine
Once you’ve had one AK, you’re more likely to get more. Prevention isn’t optional-it’s essential.
- Wear broad-spectrum SPF 50+ sunscreen every day-even in winter or on cloudy days. Reapply every two hours if you’re outside.
- Wear a wide-brimmed hat and UV-blocking sunglasses. Your ears and scalp are vulnerable.
- Avoid direct sun between 10 a.m. and 4 p.m., when UV is strongest.
- Check your skin monthly. Use a mirror to look at your back, scalp, and between your toes.
- Don’t use tanning beds. Ever.
And don’t wait for symptoms. If you’re over 40 and have spent time in the sun, get a full-body skin check once a year. In Australia, Medicare covers annual skin checks for people with a history of skin cancer or multiple AKs.
What You Can Do Right Now
You don’t need to panic. But you do need to act.
- Look at your face, neck, ears, and hands in good lighting. Run your fingers over any rough spots.
- If you find something unusual, take a photo with your phone. Compare it in a month.
- Make an appointment with a dermatologist if it’s changed, bleeds, or doesn’t fade.
- Start using sunscreen daily-even if you’re indoors most of the time. UV penetrates windows.
- Talk to your doctor about your sun exposure history. They can assess your risk level.
Actinic keratosis isn’t a death sentence. It’s a wake-up call. And if you catch it early, treatment is simple, effective, and often covered by insurance. The real cost isn’t the doctor’s visit-it’s the years of sun damage you ignored.
Can actinic keratosis go away on its own?
Sometimes, yes-but rarely. A small percentage of actinic keratoses may disappear temporarily, especially if you avoid the sun. But the underlying DNA damage remains. The lesion can come back, or new ones can appear. Relying on spontaneous healing is risky. Medical treatment removes the abnormal cells and reduces cancer risk.
Is actinic keratosis the same as skin cancer?
No, but it’s a precancer. Actinic keratosis is a precancerous lesion, meaning it has the potential to turn into squamous cell carcinoma if left untreated. Not all AKs become cancer, but because you can’t predict which ones will, doctors treat them as if they might. Early treatment prevents progression.
Do I need to worry about AK if I have dark skin?
Yes. People with darker skin tones are less likely to get actinic keratosis, but when they do, it’s often missed or misdiagnosed. Darker lesions can look like moles or age spots, delaying treatment. AK in darker skin can still progress to skin cancer. Regular skin checks are just as important for everyone.
Can sunscreen prevent actinic keratosis?
Yes, consistently. Studies show daily use of SPF 50+ sunscreen reduces new AKs by up to 50% over time. It won’t reverse existing damage, but it stops further harm. Sunscreen is your best long-term defense, especially if you’ve had AK before.
How often should I get checked for actinic keratosis?
If you’ve never had AK and are under 40 with low sun exposure, a skin check every 2-3 years is fine. If you’re over 40, have fair skin, or have had even one AK, get checked yearly. If you’ve had multiple lesions or a history of skin cancer, your dermatologist may recommend checks every 6 months.
If you’ve made it this far, you’re already ahead of most people. The next step? Look at your skin. Not just in the mirror, but with curiosity. What do you see? What’s changed? Your skin remembers every hour in the sun. Now it’s time to listen.



OMG I had no idea AK could look like a dark mole 😱 I’m South Asian and I’ve been ignoring this one spot on my cheek for years thinking it was just an age spot… time to book a derm ASAP. Thanks for the wake-up call!! 🙏🌞
While the clinical description of actinic keratosis is both accurate and clinically significant, I must emphasize that the assertion regarding the 10% progression rate to squamous cell carcinoma is derived from longitudinal cohort studies with variable follow-up intervals. The actual malignant transformation rate may be influenced by confounding variables such as immunosuppression, genetic predisposition, and cumulative UV exposure metrics, which are not uniformly accounted for in population-level epidemiological data.
Look, I’m just a guy who works outside in Texas. Sunburns? Yeah. I used to think those rough patches were just my skin being dry. Now I’m scared to look in the mirror. I’ve got three spots on my scalp and I’m bald as a cue ball. Gonna start wearing a hat. And sunscreen. Even when I’m just walking to the mailbox. No more excuses.
So let me get this straight… we’re told to slather on SPF 50 every day like it’s holy water, but the same sun that causes AK also gives us vitamin D? And the industry that profits from sunscreen also owns the dermatology clinics? And now we’re supposed to panic over every scaly patch while Big Pharma quietly laughs? 😏 I’ve got 17 AKs and I’m still alive. Maybe the real cancer is fear marketing. Just sayin’.
They don’t want you to know this, but actinic keratosis is a government bioweapon disguised as sun damage. The UV index is manipulated by satellites to target fair-skinned populations. Australia? They’ve been testing it there for decades. Dark skin? They don’t care because melanin blocks the signal. And don’t get me started on sunscreen - it’s full of aluminum nanoparticles that turn your DNA into a Wi-Fi router.
Wait… so you’re telling me I’m supposed to believe that a RANDOM patch of skin is gonna turn into CANCER… but I can still go to the beach and get a tan? And they want me to pay $300 to freeze it off? I’m not falling for it. My grandma had 47 of those and lived to 98. Maybe the real problem is the medical industrial complex selling fear like it’s a subscription box. I’m not getting it frozen. I’m gonna meditate on it. Energy healing.
AK is not a dermatological condition - it’s a socioeconomic indicator. Low-income populations in sunbelt regions are systematically denied preventive care, leading to delayed diagnosis and higher SCC mortality. The term 'sunspot' is a euphemism for institutional neglect. Topical therapies are cost-prohibitive; cryotherapy is inaccessible without insurance. This isn’t about skin - it’s about systemic inequity masked as medical advice.
Interesting how the article ignores the role of glyphosate in skin dysplasia. Studies from the Indian Journal of Dermatology (2018) show a 67% correlation between agricultural pesticide exposure and AK prevalence - yet no mention. Also, why is the focus on SPF 50? SPF 15 with zinc oxide was sufficient until the sunscreen industry redefined 'safe' to sell more. And don’t forget: UVB is essential for serotonin synthesis. Over-protection = depression. Science is being weaponized.
Let me be crystal clear - if you’re from the U.S. and you’ve lived here for more than a decade, you’ve been slowly cooked by corporate greed and government lies. They sold you cheap sunglasses, fake sunscreen, and the myth that 'you can’t get burned on a cloudy day.' And now? You’ve got AKs on your face like a walking billboard for American negligence. You didn’t get this from the sun - you got it from trusting the system. Wake up. America is a sunburn waiting to happen.
While the article exhibits commendable clinical rigor, it fundamentally fails to interrogate the epistemological hegemony of Western dermatology. The 'ABCDE rule' is a colonial construct imposed upon global skin phenotypes - particularly in the Global South, where melanin-rich epidermis operates under entirely different photobiological paradigms. One cannot diagnose a lesion through a Eurocentric lens and claim universality. The very notion of 'early detection' presupposes access to dermatologists - a luxury in Mumbai, Lagos, or Lima. This is not medicine. It’s aesthetic colonialism.