Imagine breaking out in hundreds of tiny, itchy bumps within minutes of starting a workout, walking to your car on a warm day, or even eating a spicy meal. No allergens, no new lotion, no bug bite-just heat. If this sounds familiar, you might be dealing with cholinergic urticaria, a skin condition triggered not by pollen or food, but by your own body temperature rising.
What Exactly Is Cholinergic Urticaria?
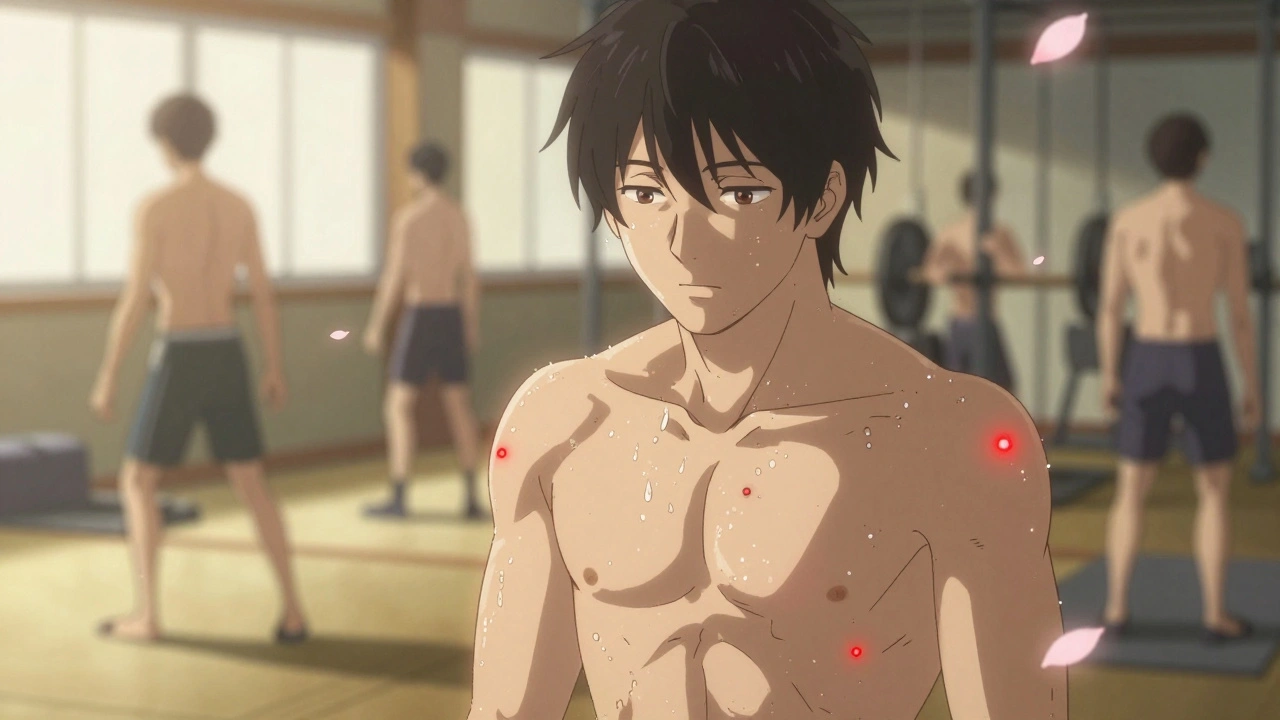
Cholinergic urticaria (CU), often called heat hives or sweat hives, is a type of physical urticaria. That means it’s not caused by an allergic reaction to something you touched or ate. Instead, it’s triggered when your body heats up-usually from sweating. When your core temperature climbs just half a degree above normal (around 37.5°C or 99.5°F), your nervous system sends a signal that mistakenly tells your skin to release histamine. The result? Tiny red bumps, usually 1-3 mm wide, surrounded by red flares. They sting, tingle, and burn more than they itch.
This isn’t just a mild rash. It’s a neuroimmune response. Research shows people with CU have lower levels of acetylcholinesterase and higher levels of certain immune signals in their sweat glands. That means your body’s own sweat becomes the trigger. And unlike hives from allergies, these bumps don’t come from contact with something foreign-they come from within.
Who Gets It and When Does It Start?
Cholinergic urticaria usually shows up in teens and young adults. Most people first notice symptoms between ages 15 and 25. It’s rare in children under 10 and less common after 40. About 5-7% of all people who get hives have this specific type. Men are slightly more likely to be affected than women, though the reason isn’t fully understood.
It’s also more common in warmer climates. In Southeast Asia, the rate is nearly four times higher than in Scandinavia. That makes sense-if you live in a hot, humid place, you sweat more often. But even in cooler places like Adelaide, where December temperatures regularly hit 30°C, CU can flare up indoors with air conditioning off or during a gym session.
What Do the Hives Look and Feel Like?
These aren’t the big, swollen welts you might picture with allergic reactions. CU hives are small-like pinpricks or goosebumps made visible. They show up fastest on areas that sweat the most: chest (78% of cases), face (65%), upper back (62%), and arms (58%). You rarely see them on your palms, soles, or inside your mouth.
The timing is precise. Symptoms start within 2-15 minutes of getting hot. They peak around 15-30 minutes after that. And they vanish just as quickly-usually within 90 minutes once you cool down. That’s why many people think it’s just a temporary reaction and don’t take it seriously. But if it happens every time you exercise, eat curry, or take a hot shower, it’s not temporary. It’s chronic.
People describe the sensation as:
- Like a hundred needles pricking your skin
- A warm, burning flush spreading across your chest
- Tingling that turns into intense itching
One Reddit user wrote: “I started running and within five minutes, my chest felt like it was on fire. I had to stop, strip off my shirt, and stand in front of a fan. It took 40 minutes for the bumps to fade.” That’s not unusual.
What Triggers Cholinergic Urticaria?
Anything that raises your body temperature can trigger it. The most common triggers, based on patient surveys, are:
- Exercise - the #1 trigger for 9 out of 10 people
- Hot weather or humid environments
- Spicy foods - capsaicin raises internal temperature
- Hot showers or baths
- Emotional stress - anxiety can cause sweating and heat buildup
- Wearing tight or non-breathable clothing
Here’s the tricky part: you can’t avoid heat entirely. Your body needs to regulate temperature. So the goal isn’t to stop sweating-it’s to manage how and when you sweat.

How Is It Diagnosed?
Doctors don’t rely on blood tests or skin prick tests for CU. Instead, they use a passive warming test. You sit in a warm room (around 39°C) or wear a heating blanket until your core temperature rises by 0.5°C. If you develop those characteristic tiny hives within 15 minutes, it’s CU. This test works in 94% of confirmed cases.
Many people are misdiagnosed. Emergency rooms often mistake CU for exercise-induced anaphylaxis. The difference? Anaphylaxis causes breathing trouble, low blood pressure, and swelling of the throat. CU rarely goes that far-but it can.
About 12% of CU patients experience systemic symptoms: dizziness, nausea, rapid heartbeat, or even wheezing. For 8.7%, this can escalate to anaphylaxis. That’s why some doctors prescribe epinephrine auto-injectors-even if you’ve never had a severe reaction before. Better safe than sorry.
What Treatments Actually Work?
There’s no cure. But most people can control symptoms with the right approach.
First-line treatment: Second-generation antihistamines
Drugs like cetirizine (Zyrtec) and loratadine (Claritin) block histamine. They’re non-drowsy, unlike older antihistamines like diphenhydramine. Most people take 10mg daily. But if that doesn’t help, doctors often increase the dose-up to 40mg of cetirizine daily. Studies show this higher dose works for 73% of patients who didn’t respond to standard doses.
Combination therapy for stubborn cases
If antihistamines alone aren’t enough, adding an H2 blocker like famotidine (Pepcid) helps. H2 blockers reduce stomach acid, but they also block a different type of histamine receptor. In one Cleveland Clinic study, 57% of patients who added famotidine 20mg twice daily saw better control.
Biologics for severe, refractory cases
In 2023, the European Medicines Agency approved omalizumab (Xolair) for CU. Originally used for asthma and chronic hives, it’s now a game-changer for people who don’t respond to anything else. In trials, 78% of CU patients on weekly 300mg doses had complete symptom relief. But it’s expensive-around $3,500 per month in the U.S.-so it’s not an option for most.
Prevention: How to Avoid Flare-Ups
Since you can’t stop your body from heating up, prevention is about control and timing.
- Work out in cool environments - Gym with AC? Better than outdoor runs. Try early morning or late evening.
- Wear moisture-wicking clothing - Avoid cotton. Look for fabrics labeled “performance,” “athletic,” or “cooling.” They pull sweat away and dry faster.
- Use cooling towels or misting bottles - Dampen a towel and drape it over your neck during exercise.
- Take antihistamines before activity - Take your daily dose 1-2 hours before working out or eating spicy food.
- Keep showers lukewarm - Hot water = trigger. Stick to warm or cool showers.
- Track your triggers - Use a free app like the Urticaria Center’s tracker. Log temperature, activity, food, and symptoms. After 2-3 months, patterns emerge. Maybe you only react after eating chili + running. Now you know to skip the curry before workouts.
One patient in the Urticaria Center’s registry said: “I used to get hives every single day. After switching to air-conditioned workouts and wearing a cooling vest, my flares dropped from daily to once or twice a month.”

When to See a Doctor
You don’t need to suffer in silence. See a dermatologist or allergist if:
- Hives appear after every heat exposure
- They last longer than 90 minutes
- You feel dizzy, short of breath, or your throat tightens
- Over-the-counter antihistamines don’t help after two weeks
Don’t wait until you have a severe reaction. If you’ve ever felt like you might pass out during a workout and broke out in hives, get checked. Epinephrine might be necessary.
The Bigger Picture: Climate Change and CU
Here’s something most people don’t talk about: climate change is making CU worse. Warmer global temperatures mean more days above 30°C. More sweating. More flare-ups. Research predicts a 15-25% increase in CU cases in temperate regions by 2040.
Companies are starting to respond. ThermaCare and Mayo Clinic are testing smart clothing that cools skin in real time. Early prototypes reduced flare frequency by 63% during exercise tests. By 2028, wearable tech that monitors your core temperature and alerts you before you overheat could become standard for CU patients.
For now, the best tools are simple: know your triggers, control your environment, and talk to your doctor. You don’t have to give up exercise. You don’t have to avoid social events. You just need a plan.
Can cholinergic urticaria go away on its own?
Yes, about 30% of people see their symptoms disappear completely within 7 to 10 years. It’s more likely to resolve in people who develop it in their teens or early twenties. But for the majority, it’s a chronic condition that requires ongoing management. Even if it doesn’t go away, most people learn to control it well enough to live normally.
Is cholinergic urticaria an allergy?
No. It’s not an allergy to anything external. Allergies involve the immune system reacting to a foreign substance like peanuts or pollen. Cholinergic urticaria is a physical reaction to heat and sweat. Your body’s own nervous system misfires, triggering histamine release. That’s why antihistamines help-but allergy shots won’t.
Can spicy food really trigger heat hives?
Absolutely. Capsaicin in chili peppers raises your internal body temperature, even if you’re not sweating. Many people with CU report flare-ups after eating curry, hot wings, or even wasabi. If you notice bumps after spicy meals, try cutting back or taking your antihistamine 30 minutes before eating.
Are there any natural remedies for cholinergic urticaria?
There’s no proven natural cure. Some people report mild relief from cool compresses, oatmeal baths, or vitamin D supplements-but these don’t stop the reaction. Antihistamines are the only treatment backed by clinical trials. Avoid unproven supplements like quercetin or stinging nettle-they’re not regulated and won’t prevent flare-ups.
Can I still exercise with cholinergic urticaria?
Yes, but you need to adapt. Avoid intense workouts in hot, humid weather. Choose low-impact activities like swimming in a cool pool, cycling indoors with AC, or yoga in a cool room. Always take your antihistamine beforehand. Keep a cold towel and water nearby. Many patients find that with the right precautions, they can stay active without flares.
Why do I get hives when I’m stressed?
Stress triggers your sympathetic nervous system, which causes sweating-even if you’re not hot. That’s enough to set off CU in sensitive people. Managing stress through breathing exercises, meditation, or even just taking breaks can reduce flare-ups. It’s not in your head-it’s a real physiological response.
Next Steps: What to Do Today
If you think you have cholinergic urticaria, start here:
- Take a photo the next time you get hives after heat exposure.
- Start a simple log: date, activity, temperature, food, symptoms, how long they lasted.
- Buy one bottle of cetirizine (10mg) and take it daily for two weeks.
- Switch to moisture-wicking workout clothes.
- If no improvement, make an appointment with a dermatologist.
You don’t need to live in fear of sweat. With the right tools, you can stay cool-literally and figuratively.




I used to think I was just bad at exercising until I started breaking out like I got poison ivy after a jog. Now I know it's heat hives. Took me 3 years and three ER trips to figure it out. Don't let them tell you it's 'just anxiety'.
The notion that this is purely a neuroimmune phenomenon ignores the broader epigenetic and autonomic dysregulation patterns observed in chronic inflammatory conditions. The acetylcholinesterase deficiency is merely a downstream biomarker, not a root cause.
If you're getting hives from heat, you're not weak. You're not lazy. You're not overreacting. This is a real medical condition. Get tested. Take the antihistamines. Wear the right clothes. Stop letting people tell you it's 'all in your head'.
I used to feel so alone with this until I found a support group. It's not just about the hives-it's the shame, the embarrassment, the fear of being judged at the gym. You're not broken. You're just wired differently. And you're not alone.
I went from never working out to doing 5Ks in the AC. I wear a cooling vest now. I carry a spray bottle. I take Zyrtec like it's my morning coffee. I used to cry after every run. Now I laugh. This isn't the end of your fitness life-it's a new level.
They don't want you to know this but the CDC is hiding the real cause. It's not sweat. It's 5G towers heating up your nervous system. They're testing this on young people so they can sell you overpriced 'smart' shirts. Wake up.
I'm from Thailand and we call this 'sweat rash' here. Everyone knows it. No one makes a big deal. We just chill in AC, drink coconut water, and wear linen. It's not a crisis-it's a lifestyle tweak. You got this 💪🌴
i had no idea spicy food could do this. i thought it was just my stomach being weird. now i know why i broke out after that thai food date. whoops. gonna skip the curry before the gym from now on 😅
i used to avoid showers after workouts because i was scared of the hives. now i take cool showers and just breathe. it's not perfect but it's better. thank you for writing this. i feel seen 🫂
i've been on cetirizine for 6 months. it's not magic but it cuts my flares in half. the trick is taking it 90 mins before working out. not right before. not after. 90 mins. trust me, i've tried it all.
The author's casual tone undermines the clinical gravity of this condition. This is not a 'quirky' skin issue-it's a dysautonomia with potential anaphylactic risk. The lack of emphasis on immunological monitoring is dangerously reductive.
so i tried the cooling vest and it felt like i was wearing a space suit. also why is everything so expensive now? like a $200 shirt to stop sweat? i just wear a tank top and deal with it
I wonder if there's a correlation between CU and low-grade chronic inflammation markers. Has anyone looked at CRP or IL-6 levels in CU patients over time? The histamine theory feels incomplete.
i started doing yoga in a cool room instead of running. no hives. no stress. just me, a mat, and peace. sometimes the best workout is the one that doesn't make you look like a boiled lobster 🙌
This isn't just about the body. It's about how we've built a culture that equates sweat with virtue. What if the problem isn't that you're overheating-but that the world refuses to accommodate natural human variation?