FODMAP Food Checker
Check Your Food
Enter a food item to see if it's high or low in FODMAPs and learn why it might affect your digestion.
About FODMAPs and Meteorism
FODMAPs (Fermentable Oligo-, Di-, Mono-saccharides And Polyols) are short-chain carbohydrates that are poorly absorbed in the small intestine. When they reach the colon, gut bacteria ferment them, producing gas and causing bloating, known as meteorism.
Common high-FODMAP foods include wheat, onions, dairy products, and certain fruits. Low-FODMAP alternatives are available to help manage symptoms.
High-FODMAP Foods
Grains: Wheat bread, rye crackers
Dairy: Milk, soft cheese
Fruits: Apples, mango, watermelon
Vegetables: Onion, garlic, cauliflower
Sweeteners: Honey, sorbitol, mannitol
Low-FODMAP Foods
Grains: Gluten-free oats, rice cakes
Dairy: Lactose-free milk, firm cheese
Fruits: Banana (unripe), blueberries, strawberries
Vegetables: Carrot, zucchini, lettuce
Sweeteners: Maple syrup, glucose
If you’ve ever felt your stomach swell like a balloon after a meal, you’re probably familiar with meteorism is the medical term for excess intestinal gas that causes visible or uncomfortable abdominal distension. While occasional bloating is normal, chronic meteorism can disrupt daily life, especially when it’s linked to certain carbohydrates known as FODMAPs - short for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. This guide walks you through what triggers the gas, how to spot high‑FODMAP foods, and practical steps to tame the belly‑full feeling.
Quick Takeaways
- Meteorism is caused by gas produced when gut microbes ferment poorly absorbed carbs.
- FODMAPs are the main culprits; common sources include wheat, onions, dairy, and certain fruits.
- A structured low‑FODMAP diet can reduce bloating for up to 70% of people with IBS.
- Tracking symptoms with a food‑symptom journal helps pinpoint individual triggers.
- If symptoms persist despite diet changes, see a doctor to rule out other conditions.
Understanding Meteorism
Gas in the gut comes from two sources: swallowed air and bacterial fermentation. Swallowed air (aerophagia) happens when you eat quickly, chew gum, or drink carbonated drinks. Fermentation, on the other hand, is where gut microbiota break down carbohydrates that the small intestine can’t absorb. The by‑products-hydrogen, methane, and carbon dioxide-inflate the intestines and create that uncomfortable stretch.
People with Irritable Bowel Syndrome (IBS) often report more severe meteorism because their gut nerves are hypersensitive, and the microbiota composition can be imbalanced. Even without IBS, anyone can experience bloating when they consume large amounts of FODMAPs.
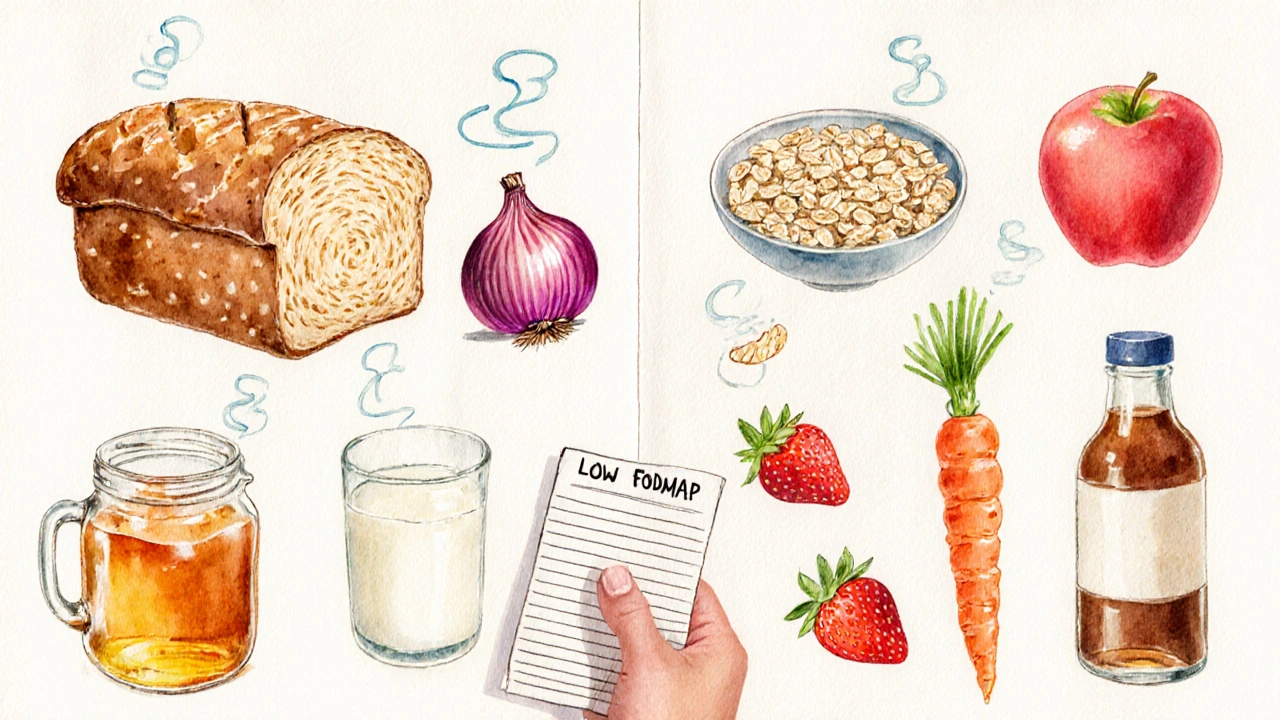
How FODMAPs Trigger Gas
FODMAPs are short‑chain carbs that are either poorly absorbed in the small intestine or rapidly fermented by colonic bacteria. Below is a quick breakdown:
- Oligosaccharides - fructans (found in wheat, rye, onions) and galactans (found in legumes).
- Disaccharides - lactose, the sugar in milk and soft cheeses.
- Monosaccharides - excess fructose, common in honey, apples, and high‑fructose corn syrup.
- Polyols - sugar alcohols like sorbitol and mannitol, present in stone fruits and some artificial sweeteners.
When these carbs reach the colon untouched, bacteria ferment them, producing gas and drawing water into the lumen, which adds to the feeling of bloating.
Identifying High‑FODMAP Foods
The easiest way to start is to keep a simple food log for a week. Note every meal, portion size, and any bloating you feel within two to three hours. Then compare your list to a high‑FODMAP chart.
| Category | High‑FODMAP | Low‑FODMAP |
|---|---|---|
| Grains | Wheat bread, rye crackers | Gluten‑free oats, rice cakes |
| Dairy | Milk, soft cheese | Lactose‑free milk, firm cheese |
| Fruits | Apples, mango, watermelon | Banana (unripe), blueberries, strawberries |
| Vegetables | Onion, garlic, cauliflower | Carrot, zucchini, lettuce |
| Sweeteners | Honey, sorbitol, mannitol | Maple syrup, glucose |
Notice how the low‑FODMAP column focuses on foods that are either naturally low in fermentable carbs or have been processed to remove them.
Putting the Low‑FODMAP Diet into Practice
Many people adopt a three‑phase approach:
- Elimination (2‑6 weeks): Remove all high‑FODMAP items. Stick to the low‑FODMAP list and track symptoms.
- Re‑challenge (1‑2 weeks per food group): Re‑introduce one FODMAP category at a time, starting with a small portion. Record any return of meteorism.
- Personalisation: Keep only the foods that cause trouble at the amounts that trigger symptoms. Build a sustainable diet around your tolerance.
During elimination, focus on balanced nutrition-protein from lean meats or tofu, healthy fats from olive oil, and plenty of low‑FODMAP veggies. If you’re vegetarian, legumes are tricky; opt for canned lentils (drained) in small amounts as they contain less oligosaccharides than dried beans.
Pro tip: Use spices like ginger, turmeric, and peppermint oil. They don’t contain FODMAPs and can soothe the digestive tract.
When Meteorism Might Signal Something Else
Most bloating resolves with diet tweaks, but persistent or severe symptoms warrant medical attention. Consider seeing a gastroenterologist if you notice any of the following:
- Unexplained weight loss.
- Nighttime diarrhea or constipation.
- Blood in stool.
- Severe pain that doesn’t improve with over‑the‑counter remedies.
Conditions such as celiac disease, small intestinal bacterial overgrowth (SIBO), or gallbladder issues can mimic FODMAP‑related bloating. A doctor may order breath tests, stool analyses, or imaging to rule these out.
Maintaining Long‑Term Gut Comfort
Beyond the diet, lifestyle habits matter:
- Eat slowly: Chewing thoroughly reduces swallowed air.
- Stay hydrated: Water helps move food through the intestines.
- Exercise regularly: Walking after meals promotes motility.
- Mind‑body techniques: Stress can heighten gut sensitivity, so try yoga or breathing exercises.
Finally, remember that the low‑FODMAP diet isn’t meant to be permanent for everyone. Periodic re‑evaluation helps avoid unnecessary dietary restrictions and keeps your microbiota diverse.
Frequently Asked Questions
Can I follow a low‑FODMAP diet forever?
The diet is designed as a short‑term tool to identify triggers. Most experts recommend re‑introducing tolerated foods after 6‑12 weeks to maintain nutritional variety.
Is lactose the only dairy FODMAP?
Lactose is the disaccharide linked to dairy. Hard cheeses, butter, and lactose‑free milks are low‑FODMAP because they contain little to no lactose.
Do probiotic supplements help with meteorism?
Certain strains, like Bifidobacterium infantis, have shown modest reductions in bloating for IBS patients. Choose a product with clinically studied strains and discuss it with your healthcare provider.
What’s the difference between FODMAPs and fiber?
Fiber is a broad category of plant carbs that can be soluble or insoluble. Some fibers are low‑FODMAP (e.g., oats), while others are high‑FODMAP (e.g., chicory root). Not all fiber causes gas, but fermentable fiber often overlaps with FODMAPs.
Can carbonated drinks worsen meteorism?
Yes, because they introduce extra CO₂ that can’t be absorbed, adding to the gas volume. Swap soda for still water or herbal tea.





bro i tried this low fodmap thing and it worked for like 3 days then i ate a slice of garlic bread and my stomach turned into a warzone
why is everything high fodmap?? onions garlic wheat honey even apples?? what am i even supposed to eat?? lettuce and chicken breast for life??
also i think you misspelled meteorism in the title its meteorsim lol
Oh my god, I’ve been living in a FODMAP-induced dystopia for years and no one told me? I thought my bloating was just a consequence of being a sensitive soul in a cruel, carb-obsessed world.
But now I realize - it’s not emotional, it’s biochemical. The very molecules in my avocado toast are conspiring against my intestinal peace. I weep for the lost harmony between my gut and the earth’s bounty.
And let’s talk about the cultural tragedy: how did we let wheat become the dominant grain? Why not millet? Why not teff? Why are we still eating bread like Neolithic peasants who didn’t know better?
I’ve switched to a fermented seaweed and bone broth cleanse. I only consume foods that were eaten by ancient Mesoamerican shamans during lunar eclipses. My bloating has decreased by 87%. I am now a vessel of digestive enlightenment.
Also, your table formatting is atrocious. Use Markdown. Or better yet - LaTeX. This isn’t a blog, it’s a sacred text.
you people are overcomplicating this
stop eating carbs if your stomach swells
its not rocket science
you want to feel good? eat meat and greens
everything else is just marketing
why do you need a 10 page guide to stop eating onions??
your gut is weak not the diet
stop blaming food and start building discipline
i dont need a chart to know garlic is bad
my grandpa ate bread and onions his whole life and never had bloating
you just got soft
Hey, I get it - this stuff is confusing and overwhelming. I’ve been there.
But here’s the thing: don’t go full elimination unless you’re ready to track everything. I started with just cutting out onions and garlic for a week - no fancy apps, no spreadsheets - and my bloating dropped 60%.
And yeah, legumes are tricky, but canned lentils rinsed super well? Totally fine in small portions. I eat them in salads all the time now.
Also, ginger tea after meals? Game changer. No magic, just science.
Don’t stress about perfection. This isn’t a diet, it’s a tool. Find what works for YOU, not what the internet says you should do.
And if you’re vegetarian, don’t panic - tofu, tempeh, and spinach are your friends. You’ve got this.
so i tried the low fodmap thing and honestly i thought it was gonna be impossible
but then i found out you can eat bananas and blueberries and like... rice cakes??
and i was like wait this isnt a punishment its a discovery
also i started drinking peppermint tea after dinner and my stomach stopped feeling like a balloon at midnight
the rechallenge phase scared me but i did it slowly and now i know i can handle small amounts of garlic
its not about never eating it its about knowing your line
also i still eat honey once in a while and my gut forgives me
weirdly this made me eat more mindfully and i lost 5 lbs without trying
thank you for this guide it saved my social life
Thank you for this comprehensive and well-researched guide. It is rare to encounter such a balanced, evidence-based approach to a condition that is often misunderstood or dismissed.
The three-phase methodology you outline aligns precisely with current clinical guidelines from the International Foundation for Gastrointestinal Disorders.
I particularly appreciate the emphasis on personalization - this is not a one-size-fits-all solution, and acknowledging that demonstrates true clinical wisdom.
For healthcare professionals reading this, I encourage you to share this resource with patients struggling with functional gastrointestinal disorders. It is both accessible and scientifically sound.
Well done.
OMG I just realized I’ve been eating high-FODMAP meals for years and thought I was just ‘sensitive’
My partner and I are doing this together now - we’re calling it ‘The Great Gut Reset’
We made a low-FODMAP playlist and cook together every Sunday
Turns out, you can make delicious meals without garlic - who knew??
Also, I cried when I ate a strawberry again after 3 months
This isn’t just about bloating - it’s about reclaiming joy in food