HIV Test Window Period Calculator
Calculate Your Test Timing
Get accurate guidance on when to test based on your exposure type and test method.
Results will appear here
Missing an early chance to know your HIV status can cost you health, peace of mind, and future options. early HIV detection lets you start treatment before the virus does too much damage and reduces the chance of passing it on. This guide explains why a simple HIV‑1/2 test right now is one of the smartest health moves you can make.
What Is an HIV-1/2 Test?
HIV-1/2 test is a screening method that detects antibodies to HIV‑1 and HIV‑2, or the virus’s genetic material, to determine if a person is infected. The test comes in several formats: rapid point‑of‑care kits that give results in 20 minutes, laboratory‑based ELISA that may take a day, and home‑collection kits that you send to a lab.
Why Early Detection Saves Lives
- Antiretroviral therapy (ART) is most effective when started within weeks of infection; it can keep the viral load undetectable and protect the immune system.
- Knowing your status early cuts the chance of unknowingly transmitting HIV to partners.
- Early diagnosis reduces long‑term healthcare costs by preventing opportunistic infections.
- Psychological relief comes from having answers, whether the result is negative or positive.
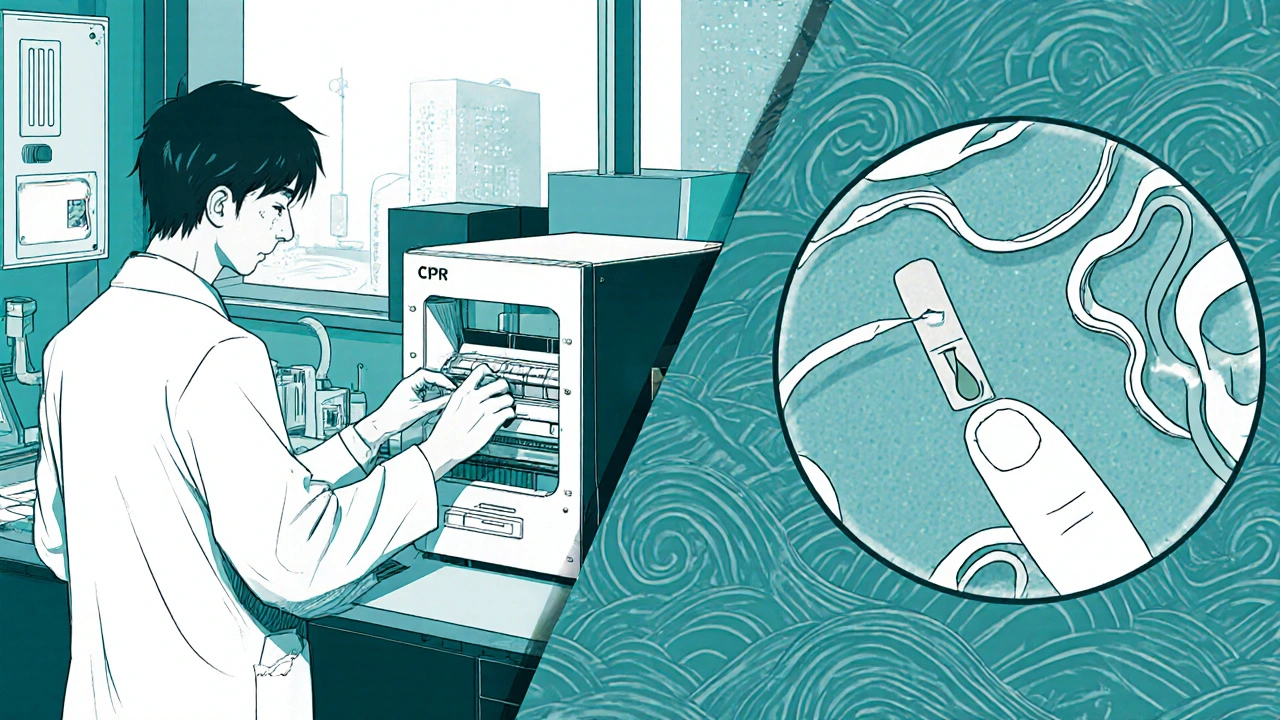
How the Test Works: From Sample to Result
- Sample collection - a finger‑prick blood drop for rapid tests or venous blood/ oral fluid for laboratory tests.
- Detection method - ELISA looks for antibodies, while PCR amplifies viral RNA to catch infection earlier.
- Result timing - rapid tests show results in 15‑30 minutes; lab tests usually within 24‑48 hours.
- Follow‑up - a positive rapid test is confirmed with a lab‑based test; a negative result during the "window period" may need re‑testing after 3 weeks.
Choosing the Right Test for You
| Feature | Rapid Test | Lab‑Based ELISA | Home Testing Kit |
|---|---|---|---|
| Result Time | 15‑30 minutes | 1‑2 days | 3‑7 days (mail‑in) |
| Sample Type | Finger‑prick blood or oral fluid | Venous blood | Oral fluid or finger‑prick |
| Detection Window | 3‑4 weeks | 2‑4 weeks | 3‑4 weeks |
| Cost (USD) | $20‑$40 | $50‑$100 | $30‑$60 |
| Need for Confirmation | Yes, if positive | No (standard) | Yes, if positive |
If you need immediate peace of mind, a rapid test at a clinic or pharmacy is best. For the most accurate diagnosis, especially if you’re in the early window period, a lab‑based ELISA or PCR is recommended. Home kits offer privacy and convenience, but remember a positive result still requires professional confirmation.
Understanding Key Health Metrics After a Positive Result
- CD4 count: measures immune system strength; a count above 500 cells/µL is considered healthy.
- Viral load: the amount of HIV RNA in blood; undetectable (< 50 copies/mL) means treatment is working.
- Resistance testing: determines if the virus is resistant to certain antiretroviral drugs, guiding the optimal regimen.
These numbers guide your healthcare provider’s choice of antiretroviral therapy and help track progress over time.
Common Myths That Stop People From Testing
- "I’m not at risk" - HIV can be transmitted through unexpected exposures; many infections occur in people who thought they were low‑risk.
- "The test is painful" - finger‑prick tests feel like a quick pinch; oral swabs are painless.
- "If I test positive, I’ll be judged" - stigma is real, but many clinics offer confidential, non‑judgmental services.
- "Treatment isn’t effective" - modern ART can suppress the virus to undetectable levels in >95% of patients.
Dispelling these myths makes it easier to get tested early.
Where to Get an HIV‑1/2 Test in 2025
- Community health centres - often free or low‑cost. \n
- Pharmacies - many carry rapid tests that a pharmacist can administer.
- Online providers - order a home kit, collect the sample, and mail it to a certified lab.
- Hospitals - for comprehensive testing and immediate linkage to care if positive.
In Australia, the government funds free testing at many locations, and the “HIV Test‑Now” app can locate the nearest drop‑in service.
Next Steps After a Negative or Positive Result
If negative: consider retesting after the window period if you had a recent exposure, and keep practicing safer sex.
If positive: schedule a confirmatory appointment within a week, start discussing ART options, and inform any recent partners so they can test as well.
Both outcomes are an opportunity to take control of your health.
Key Takeaways
- Early testing catches HIV before serious immune damage occurs.
- Rapid, lab‑based, and home tests each have pros; choose based on speed, accuracy, and privacy needs.
- Positive results lead to effective ART that can make the virus undetectable.
- Testing is widely available and often free; don’t let myths stop you.
- Follow up promptly-whether the result is negative or positive-to stay healthy.
How soon after exposure can I get a reliable HIV‑1/2 test?
A rapid test can detect antibodies reliably after 3‑4 weeks, but a lab‑based PCR can pick up the virus as early as 10 days. Re‑testing at 3 weeks and again at 6 weeks is safest if you’re unsure.
Are HIV‑1/2 tests confidential?
Yes. Clinics, pharmacies, and online services all follow privacy laws. In many regions, results are not linked to your name unless you give consent.
What is the difference between HIV‑1 and HIV‑2?
HIV‑1 is the most common worldwide, while HIV‑2 is less transmissible and mostly found in West Africa. Most tests detect both, but some regions may use specific assays for HIV‑2.
Can I test myself at home?
Yes. Home kits use oral fluid or a finger‑prick. If the result is positive, you’ll need a confirmatory lab test, which most providers arrange for free.
What happens after a positive diagnosis?
You’ll meet a healthcare team to start antiretroviral therapy, get baseline CD4 and viral‑load tests, and receive counseling on treatment adherence and partner notification.




Skipping the test is stupid; get tested now.
It is a civic duty to know your status; early detection protects you and your community. By getting tested promptly, you contribute to public health and reduce transmission risks. Ignoring this responsibility undermines the collective effort to combat HIV.
Did you ever notice how every clinic claims "confidentiality"... yet data can be leaked, traced, and used against you??? The powers that be want your blood, your info, your silence!!! Beware the hidden agendas behind those friendly pamphlets!!!
Listen up, folks, because this is important! Early testing isn’t just a suggestion, it’s a lifesaver. When you get your results quick, you can start treatment before the virus does major damage. The sooner you start ART, the better your immune system can bounce back. It also means you’re less likely to pass the virus on to anyone you care about. People often think a quick finger‑prick is painful, but it’s just a tiny pinch-nothing compared to the long‑term battle you avoid. You might feel anxious waiting for results, but remember, knowledge is power and peace of mind. If you’re in the window period, don’t panic-just retest after a few weeks; a negative now doesn’t guarantee you’re clean forever. The cost differences between rapid tests and lab tests are worth it when you consider the health savings later. Also, home kits give privacy, but a positive result still means you’ll need professional follow‑up. Trust the system that has helped millions live healthy lives. Don’t let stigma stop you from taking this simple step. It’s a small effort for a huge return-think of all the future plans you can keep making. So grab a test, get the facts, and move forward with confidence! Remember, the fight starts with a single drop of blood.
The whole push for universal testing feels like another wave of control, a narrative to label everyone and strip away personal freedom. Real empowerment comes from questioning authority, not blindly following health mandates. The market for rapid tests is booming, and that profit motive can’t be ignored.
Oh great, another reminder to get a finger prick, because we all have endless free time to stare at a tiny drop of blood.
💔 I can feel the weight of every missed test, the silent dread that haunts us all. 🌪️ It’s like a storm inside, waiting to burst, and only a simple test can calm the chaos. 🎭 Don’t let fear cage you; take that step and breathe.
Testing early is a simple step toward a healthier future.
Facts show that early ART improves outcomes dramatically.
Ignoring your health is selfish and avoidable.
While the impulse to resist can feel empowering, true freedom often lies in informed choice rather than blind defiance. Knowledge equips us to make decisions that honor both personal autonomy and collective well‑being.
Consider the hidden networks that profit from our fear, the silent agreements between pharma giants and policy makers that turn health into commodity. When we accept the narrative without scrutiny, we become cogs in a machine designed to monitor and control. Early testing, dressed as benevolence, can also be a surveillance tool, feeding data into systems that track our movements and choices. The moral high ground claimed by health campaigns often masks ulterior motives, and those who speak out are labeled conspiratorial. Yet history teaches us that vigilance is essential; without it we surrender our privacy and agency. The push for universal testing must be examined not just for its medical merits but for the power structures it reinforces. By questioning, we protect ourselves from unseen exploitation. Remember, the path to true health includes freedom from manipulation, not just clinical outcomes.