Vitamin K Consistency Calculator
Daily Vitamin K Tracker
Track your vitamin K intake to maintain stable INR levels. Consistency is key—not avoidance.
Your Daily Vitamin K Intake
When you're on warfarin, your diet isn't about cutting out healthy foods-it's about keeping things steady. Many people think they need to avoid spinach, kale, or broccoli because they've heard these foods interfere with their blood thinner. That’s not true. What actually matters is consistency. Eating the same amount of vitamin K every day helps your warfarin work the way it should, without dangerous spikes or drops in your INR.
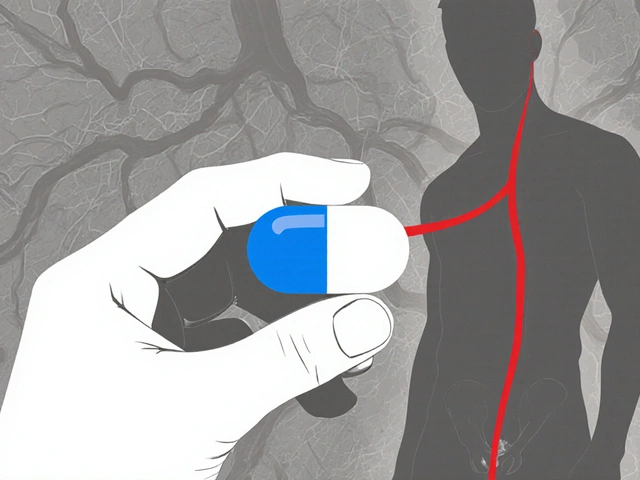
Why Vitamin K Matters with Warfarin
Warfarin works by blocking vitamin K’s role in making blood clotting proteins. Without enough vitamin K, your blood takes longer to clot-which is exactly what you want if you’re at risk for strokes or clots. But here’s the catch: if you suddenly eat a lot more vitamin K than usual, your body gets enough to make those clotting proteins again. That makes warfarin less effective. Your INR drops, and your risk of clotting goes up. On the flip side, if you eat way less vitamin K than normal, your INR shoots up, raising your risk of bleeding.The numbers don’t lie. Studies show that a 100 mcg increase in daily vitamin K intake can lower your INR by 0.5 to 1.0 points. For someone with a target INR of 2.5, that’s the difference between being protected from clots and being dangerously under-anticoagulated. And it doesn’t take much to throw things off. One extra cup of cooked kale or a big bowl of raw broccoli can do it.
Which Foods Have the Most Vitamin K?
Vitamin K1 (phylloquinone) is the main form in food, and it’s mostly found in green leafy vegetables. Here’s what’s packed with it:- Cooked kale: 1,062 mcg per cup
- Cooked spinach: 889 mcg per cup
- Raw Swiss chard: 299 mcg per cup
- Cooked Brussels sprouts: 156 mcg per cup
- Raw broccoli: 85 mcg per cup
- Asparagus: 70 mcg per cup
- Green tea: 41-88 mcg per serving
Other sources include soybean oil, canola oil, and some fermented foods like natto (which has vitamin K2), but those are less common in most diets. The key isn’t to avoid these foods-it’s to know what you’re eating and keep your portions steady.
Consistency Over Restriction
You don’t need to stop eating greens. In fact, the American Heart Association, the Anticoagulation Forum, and the Mayo Clinic all say the same thing: don’t avoid vitamin K, just keep it consistent.Think of it like this: if you normally eat one cup of cooked spinach three times a week, keep doing that. Don’t switch to three cups one week because you’re trying to eat healthier. Don’t skip them entirely because you’re afraid of your INR rising. Your body adapts to your routine. Fluctuations are what mess with your warfarin-not the vitamin K itself.
Research shows that patients who keep their daily vitamin K intake within 20% of their usual amount stay in their target INR range 78% of the time. Those with wild swings? Only 42%. A 2019 study found that people who got personalized diet advice had 37% fewer out-of-range INR tests over six months.

Real-Life Triggers That Throw Off INR
Patients report the most trouble with:- Seasonal changes-spring brings fresh greens, winter doesn’t
- Starting a new “clean eating” or vegan diet full of kale and broccoli
- Eating out-restaurant salads can have double or triple the greens you’d use at home
- Skipping meals or fasting
- Switching brands of multivitamins (some have vitamin K, others don’t)
One patient on Reddit saw his INR drop from 2.8 to 1.9 after eating three kale salads in a row during a detox. He needed a 15% warfarin dose increase. Another patient kept her INR stable for eight years by eating exactly two cups of cooked spinach every Tuesday and Thursday. No more, no less.
How to Stay on Track
Here’s what actually works:- Measure your greens. Don’t guess. Use a measuring cup. A cup of cooked spinach isn’t the same as a handful. Be precise.
- Track your intake. Keep a simple food log. Note the day, the food, and the portion. You don’t need an app-just a notebook. Review it with your doctor or anticoagulation clinic every visit.
- Stick to your routine. If you eat spinach on Tuesdays and Thursdays, do it every week. If you don’t eat it at all, don’t start suddenly.
- Check your multivitamin. If you take one, make sure it has the same amount of vitamin K every time. Switching brands can cause INR swings.
- Plan ahead for eating out. Ask for dressing on the side. Skip the extra greens. Order grilled chicken with steamed vegetables instead of a big salad.
- See a dietitian. If you’re struggling, ask your doctor for a referral to a registered dietitian who specializes in anticoagulation. Patients who do this stay in range 85% of the time-compared to 65% with standard care.
What About Supplements and Other Vitamins?
Avoid herbal supplements like ginkgo, garlic, ginger, or green tea extract-they can interact with warfarin. Even “natural” doesn’t mean safe.If you take a multivitamin, keep the same brand and dose. Some have 20-50 mcg of vitamin K. Others have none. That inconsistency can be just as risky as eating too much kale.
Also, don’t start taking vitamin K supplements unless your doctor tells you to. They’re not a fix for low INR-they’re a tool for emergencies, like when your INR is dangerously high.
What to Do If You Eat Too Much Vitamin K
If you accidentally eat a huge amount-like a giant salad with kale, spinach, and broccoli-you don’t need to panic. But you should tell your anticoagulation clinic. They might suggest a small dose increase the next day, usually 10-20% higher than your normal dose. Never adjust your warfarin on your own.If your INR goes above 10 (without bleeding), your doctor may give you 1-2.5 mg of oral vitamin K to bring it down safely. This isn’t a daily fix-it’s a medical intervention.
The Bigger Picture: Why This Matters
Warfarin isn’t outdated. It’s still used by over 2.6 million Americans every year because it’s cheap, reversible, and well-understood. Newer blood thinners exist, but they’re not always the right choice-especially for people with mechanical heart valves or kidney problems.And here’s something surprising: research now suggests that consistent moderate vitamin K intake (75-100 mcg/day) may actually improve warfarin stability better than very low intake. Why? Because your body has a steady supply to work with. It’s not about deprivation-it’s about balance.
Your job isn’t to be perfect. It’s to be predictable. Your body learns your rhythm. If you eat the same amount of vitamin K every day, your warfarin dose can stay steady. That means fewer blood tests, fewer dose changes, and less worry.
Final Thought: You’re in Control
The CDC says it best: “It’s up to you to decide how much vitamin K you choose to eat… just keep it about the same amount each day.”You’re not a patient who has to follow rigid rules. You’re someone who’s learning how to live well with a medication that works best when your life stays steady. Eat your greens. Enjoy your broccoli. Just don’t suddenly double it. And if you’re unsure? Talk to your doctor or a dietitian. Small, consistent choices make all the difference.


I swear, I ate a giant kale smoothie last week and my INR dropped to 1.2 like it got hit by a truck 😩
Now I’m scared to even look at greens. I miss my salads.
Why does my body have to be this dramatic??
Also, why is everyone so chill about this? I feel like I’m the only one crying over broccoli.
Consistency is king. I’ve been on warfarin for 7 years. I eat exactly 1 cup of cooked spinach every Tuesday and Thursday. No more, no less.
Didn’t change a thing. No freakouts. No panic. Just steady.
You don’t need to be perfect-you just need to be predictable. Your body learns your rhythm. It’s that simple.
It’s fascinating how such a simple concept-consistency-can be so profoundly effective in medicine.
Most people think treatment means restriction or elimination, but here the solution is integration, not avoidance.
Our bodies aren’t broken machines to be fixed; they’re systems that thrive on rhythm.
Maybe this is a metaphor for life too-stability doesn’t come from avoiding change, but from anchoring yourself in small, repeatable patterns.
It’s quiet wisdom, really. Not flashy, not trendy-but deeply human.
Let me be perfectly clear: this article is dangerously oversimplified.
There is no such thing as "consistent" vitamin K intake when restaurants, seasonal produce, and unregulated supplements are involved.
And yet, the medical establishment continues to push this myth that patients can control this with a measuring cup.
What about the elderly? The visually impaired? The ones who can’t afford organic kale or don’t have time to log meals?
This isn’t patient empowerment-it’s patient blame dressed up as advice.
Oh wow, another one of those "just eat the same greens every day" posts.
Did you know that vitamin K content varies by soil, harvest time, and cooking method? A cup of "cooked spinach" from Trader Joe’s isn’t the same as from Whole Foods or your neighbor’s garden.
And what about gut bacteria? Some people metabolize K differently.
And don’t even get me started on how warfarin’s half-life changes with liver function, hydration, alcohol, or even your menstrual cycle.
So no, you can’t just "measure your greens" and call it a day. That’s textbook medical reductionism.
And yet, here we are, pretending this is a diet problem, not a pharmacokinetic one.
Pathetic.
For anyone feeling overwhelmed: you’re not alone. I started tracking my greens with a notebook and a ruler-yes, a ruler. I measure the height of the pile in the cup.
It sounds silly, but it worked.
I went from 3 out-of-range INRs in 3 months to 1 in 8 months.
You don’t need to be perfect. You just need to be aware.
And if you’re struggling, ask for a dietitian. Seriously. They’re not a luxury-they’re part of your care team.
You deserve to live without fear. Small steps, not giant leaps.
Let’s be real-this whole "vitamin K consistency" thing is just a distraction from the fact that warfarin is a 70-year-old drug with a 20% failure rate.
Why are we still forcing patients to become nutritionists when we have DOACs that don’t care what you eat?
Because Big Pharma doesn’t make enough money off warfarin.
And because doctors are too lazy to switch.
And now they’re making you feel guilty for wanting to eat a salad.
It’s not your fault. It’s the system.
And if you’re still on warfarin? You’re not failing-you’re surviving a broken healthcare model.
And that’s not empowering-it’s exploitation wrapped in a measuring cup.
It is not scientifically accurate to suggest that "eating the same amount of vitamin K every day" guarantees INR stability.
Studies show that individual variability in vitamin K absorption, gut microbiome composition, and CYP2C9 polymorphisms account for up to 40% of INR fluctuation.
Therefore, dietary consistency is merely a contributing factor, not a primary control mechanism.
Furthermore, the assertion that "your body adapts to your routine" is biologically misleading.
The liver does not "learn"-it metabolizes.
And the notion that a notebook is sufficient for clinical management is dangerously naive.
One must utilize pharmacogenomic testing and INR trend analysis, not culinary diary-keeping.
This article is a disservice to public health.
You think you’re in control because you measure your spinach?
What about the pesticides? The mold? The glyphosate in your kale?
And what if your water has fluoride? It binds to vitamin K.
And your multivitamin? Maybe it’s fake.
Maybe your INR isn’t dropping because of greens-it’s dropping because the government is controlling your blood through the food supply.
They want you dependent. They want you measuring. They want you afraid.
Stop eating their greens.
Stop measuring their cups.
Start questioning everything.
They’re lying. Vitamin K doesn’t affect warfarin. It’s the fluoride in the water that’s lowering your INR.
And the spinach? It’s just a distraction.
Don’t believe the hype.
Check your tap.
They know.