When pain becomes constant, it’s easy to spiral. You start thinking, "This will never get better," "I can’t handle this," or "Something terrible is happening inside me." These aren’t just thoughts-they’re patterns. And they make the pain worse. This is called pain catastrophizing. It’s not about being weak or overly dramatic. It’s a real psychological response that science has studied for decades. The good news? You can change it. And one of the most effective ways is through cognitive behavioral therapy (CBT).
What Exactly Is Pain Catastrophizing?
Pain catastrophizing is when your mind gets stuck on pain-ruminating on it, blowing it out of proportion, and feeling completely helpless. It’s not the physical injury itself that causes the worst suffering-it’s what you tell yourself about it. Researchers break this down into three clear parts:
- Rumination: You can’t stop thinking about the pain. It loops in your head like a broken record.
- Magnification: You assume the worst. "This ache means I’m getting worse," or "This could lead to paralysis."
- Helplessness: You feel like there’s no way out. "Nothing helps. I’m stuck like this forever."
The Pain Catastrophizing Scale (PCS) is the standard tool used to measure this. It’s a 13-question survey where people rate how often they think these thoughts. A score of 30 or higher means you’re in the clinically significant range. That doesn’t mean you’re broken-it means your brain has learned a pattern that’s making your pain more intense.
How CBT Breaks the Cycle
CBT doesn’t try to erase pain. It doesn’t promise a cure. What it does is help you separate what’s happening in your body from what’s happening in your mind. Think of it like untangling two wires that got stuck together. One wire is physical pain. The other is catastrophic thinking. When they’re tangled, they feed each other. CBT helps you untangle them.
Here’s how it works in practice:
- Self-monitoring: You start tracking your thoughts. Not just "I hurt," but "When I stood up, I thought, ‘This will ruin my day,’ and then I sat back down and didn’t move for an hour." Writing it down helps you see the pattern.
- Cognitive restructuring: Once you notice the thought, you learn to challenge it. Instead of "I can’t do anything," you ask: "What’s the evidence? Have I done anything today despite the pain? What’s a more realistic thought?"
- Behavioral activation: You start doing small things you’ve been avoiding-not because the pain is gone, but because you’re learning you can still move through it. Even 10 minutes of walking or washing dishes counts.
One study followed a 45-year-old woman with fibromyalgia. Her PCS score was 42-severe catastrophizing. After 12 weeks of CBT, it dropped to 18. Her pain intensity fell by half. She went back to part-time work. She didn’t become pain-free. But she stopped letting pain control her life.
Why CBT Works Better Than Other Approaches
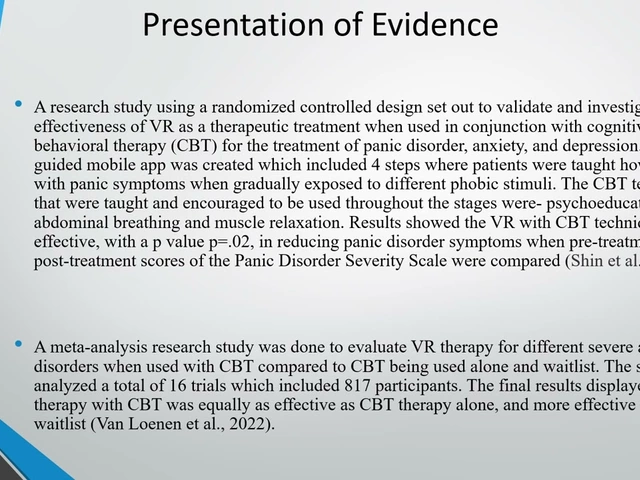
There are lots of treatments for chronic pain: meditation, acupuncture, exercise, drugs. But when it comes to specifically reducing catastrophizing, CBT stands out. A major review by the International Association for the Study of Pain found that CBT had nearly twice the effect size compared to other therapies targeting catastrophizing. Even better? When CBT is combined with gentle movement or physical therapy, the results jump even higher.
Other therapies like Acceptance and Commitment Therapy (ACT) help too, but they’re not as focused on changing the thought patterns that fuel catastrophizing. CBT is direct. It gives you tools to spot, stop, and shift those thoughts. And it’s backed by brain imaging: when people reduce catastrophizing, activity drops in areas of the brain linked to fear and threat detection.
What to Expect in a CBT Program
Most structured CBT programs for pain last 8 to 12 weeks. Sessions are usually once a week, 60 minutes long. The first few weeks are about awareness. You learn what catastrophizing looks like in your own life. By week 4, you start practicing thought replacement. By week 8, you’re applying it in real situations-like going to the grocery store or getting out of bed on a bad day.
You don’t need to be a therapist to do this. Many VA hospitals, pain clinics, and even apps now offer CBT-based programs. The Veterans Health Administration has made pain catastrophizing screening mandatory since 2020. They’ve seen 32% average reductions in PCS scores among participants. Digital tools like Curable and PainScale have over 450,000 active users as of early 2024. These aren’t just apps-they’re guided programs built on the same principles as in-person CBT.
Challenges and Real-Life Barriers
CBT isn’t magic. It’s work. And when you’re in pain, your mental energy is low. Some people say: "When my pain is an 8 out of 10, I can’t even think clearly, let alone reframe my thoughts." That’s real. And it’s why CBT works best when you start early-before the pain becomes overwhelming.
Another common issue is impatience. People expect quick fixes. But CBT takes time. The average dropout rate is around 22%. Those who stick with it? 78% report meaningful reductions in distress. Success isn’t about eliminating pain. It’s about reclaiming control.
One Reddit user wrote: "CBT helped me recognize when I’m catastrophizing. Now when I think, ‘I’ll never walk again,’ I pause and say, ‘That’s not true. I walked to the kitchen yesterday.’" That’s the power of small shifts.

Who Benefits Most?
CBT works best for people who:
- Have chronic pain (fibromyalgia, back pain, arthritis, etc.)
- Are willing to track their thoughts and behaviors
- Have some mental bandwidth to engage in reflection
- Are not in the middle of a severe depression or anxiety episode (those need separate treatment first)
People with higher education levels tend to do better, likely because they’re more familiar with reflective thinking. But that doesn’t mean others can’t benefit. It just means they might need more support, simpler language, or slower pacing.
The Bigger Picture
Pain catastrophizing isn’t just about feeling bad. It’s linked to higher rates of depression, sleep problems, and even suicidal thoughts in chronic pain patients. That’s why major health systems now screen for it. By 2025, 75% of pain clinics in the U.S. will include it in routine care. The VA, hospitals, and private clinics are all moving in the same direction.
And it’s not just about therapy. Researchers are testing smartphone apps that deliver CBT micro-interventions in real time-when you’re having a catastrophizing moment. Imagine getting a gentle nudge on your phone: "You’re having a catastrophizing thought. What’s one thing you did today despite the pain?" That’s the future-and it’s already being tested.
The goal isn’t to think positively. It’s to think accurately. Pain is real. Suffering is optional. CBT doesn’t take away your pain. It takes back your power.
Is pain catastrophizing the same as being anxious about pain?
Not exactly. Anxiety about pain is a general feeling of worry or fear. Pain catastrophizing is more specific: it’s a pattern of thinking that includes rumination (repeating negative thoughts), magnification (blowing pain out of proportion), and helplessness (feeling unable to cope). You can be anxious without catastrophizing-but catastrophizing almost always includes anxiety.
Can I do CBT for pain catastrophizing on my own?
Yes, but it’s harder. Self-guided CBT using apps like Curable, PainScale, or free resources from the VA Whole Health Library can help. Many people report success. But working with a trained therapist-especially early on-increases your chances. A therapist helps you spot blind spots, correct distorted thinking, and stay consistent when motivation drops.
How long until I see results from CBT?
Most people start noticing changes in 4 to 6 weeks. That’s when they begin to recognize their catastrophic thoughts automatically. Meaningful reductions in distress and pain intensity usually show up by week 8 to 12. It’s not overnight, but it’s lasting.
Does CBT work for everyone with chronic pain?
No. CBT is most effective for people whose pain is worsened by negative thinking patterns. If someone has severe depression, untreated PTSD, or active substance use, those issues need to be addressed first. CBT for pain catastrophizing isn’t a cure-all-it’s a tool for a specific part of the pain experience.
What if I can’t afford CBT therapy?
Many public health systems, including the VA in the U.S., offer free CBT for chronic pain. Online programs like Curable and PainScale have affordable monthly plans. Libraries and community centers sometimes host free pain management workshops. You don’t need expensive care to start. Even journaling your thoughts for 10 minutes a day can begin to shift the pattern.




Pain is not just a sensation. It's a metaphysical rupture. When the body screams, the mind doesn't just react-it reconstructs reality. Catastrophizing isn't irrational. It's the soul's last defense against meaninglessness. CBT tries to patch the fracture with logic, but logic can't hold back the tide of existential dread. The real question isn't whether thoughts can be reframed-it's whether we're willing to sit with the silence after the narrative collapses.
CBT is just corporate wellness theater. They sell you a 12-week program like it's a gym membership for your brain. Meanwhile your pain is still there. And now you feel guilty for not 'reframing' it right. Real pain doesn't care about your thought logs.
I want to say thank you for writing this. So many people think chronic pain is just 'in your head'-but you showed how the head can become a prison. The part about small actions-washing dishes, walking to the kitchen-that’s the heartbeat of recovery. You don’t need to fix everything. Just show up for one tiny thing. That’s courage.
The VA’s mandatory screening is quietly revolutionary. We’ve spent decades treating pain as a purely physiological problem. Now we’re admitting that the mind’s echo matters as much as the nerve’s fire. This isn’t soft science. It’s neurobiology meeting lived experience. And for once, the system is catching up to the patients.
i just wanted to say i read this and cried a little. not because i’m sad but because for the first time in 7 years someone described exactly what it feels like to be stuck in that loop. the rumination, the magnification, the helplessness. i didn’t know it had a name. now i know it’s not just me being weak. thank you.
Oh wow. CBT. Because clearly what chronic pain patients need is one more thing to fail at. Next they’ll be selling mindfulness subscription boxes. Let’s monetize suffering. Again.
Life is suffering. That’s the first truth. But suffering without meaning? That’s the true curse. Pain catastrophizing is the ego’s refusal to bow to impermanence. CBT? It’s not about changing thoughts-it’s about dissolving the illusion that the thinker must control the thought. The moment you stop fighting the spiral… you stop feeding it. That’s not therapy. That’s enlightenment.
my mom had fibro for 20 years. tried everything. meds, acupuncture, yoga, even a weird energy healer in Oregon. the only thing that gave her back some life was sitting down with a notebook and writing out her catastrophic thoughts. not to fix them. just to see them. like, 'oh. there’s that story again.' weirdly simple. weirdly powerful.
This is why India needs to stop copying Western therapy fads. Pain is a test of character. We used to endure. We don’t need to 'restructure thoughts.' We need discipline. Hard work. Spiritual strength. CBT is a crutch for the emotionally lazy.
I’m 3 weeks into a self-guided CBT app. Yesterday I stood in the grocery line and my knee screamed. Instead of thinking 'I’ll never be able to do this again' I just whispered 'I’m here. I’m still here.' And I kept standing. It didn’t fix the pain. But it fixed something else. I’m not giving up. Not today.
I’ve been in chronic pain for 14 years. I’ve tried every app, every therapist, every journal. The only thing that worked? Quitting. Quitting the fight. Quitting the hope. Quitting the need to 'fix' it. Pain isn’t your enemy. Your obsession with escaping it is.