Myeloma Immunotherapy Comparison Tool
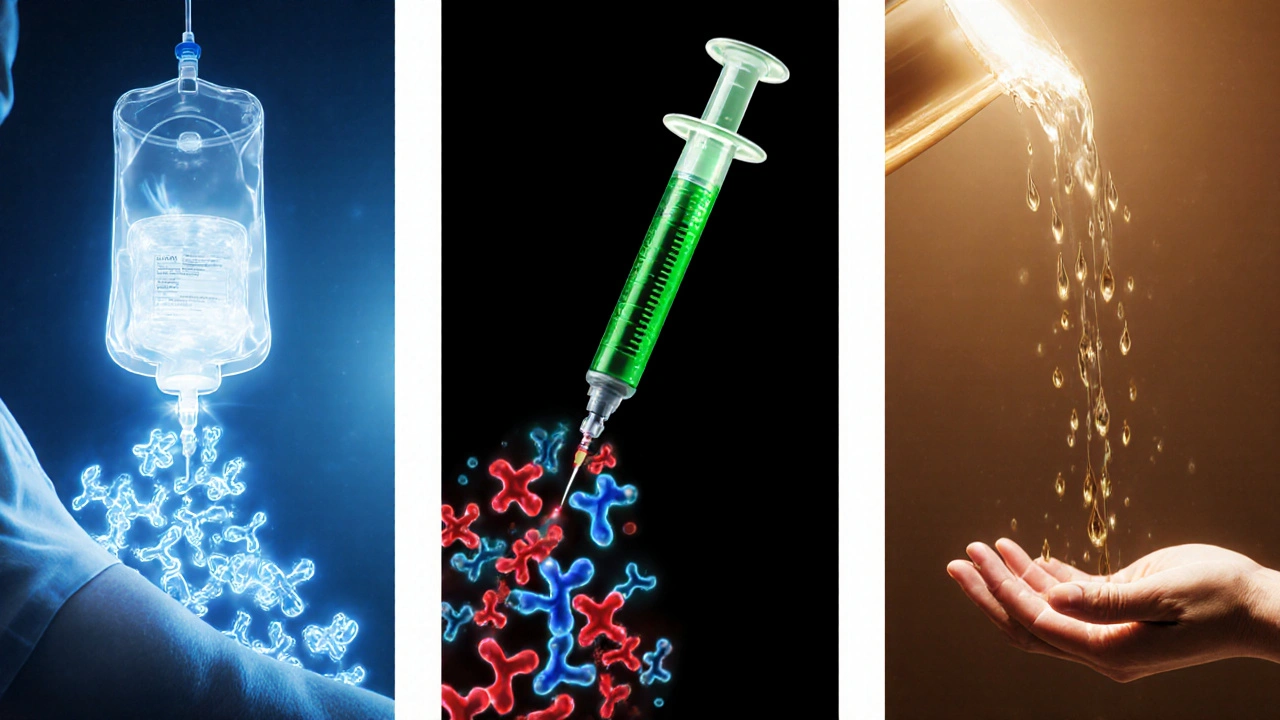
CAR T-Cell Therapy
Engineered T-cells targeting BCMA
Bispecific Antibodies
Bridge between tumor and T-cells
Checkpoint Inhibitors
Releases immune inhibition
Detailed Comparison
| Feature | CAR T-Cell | Bispecific | Checkpoint Inhibitor |
|---|---|---|---|
| Mechanism | Engineered T-cells bind BCMA | Binds BCMA + CD3 to form bridge | Blocks PD-1/PD-L1 interaction |
| Approval Year | 2021-2022 | 2022 | Not FDA approved |
| Response Rate | ≈80% overall, 40% CR | ≈63% overall, 40% CR | Modest as monotherapy |
| Administration | Single infusion after lymphodepletion | Weekly SC injections | IV every 3 weeks |
| Side Effects | CRS, neurotoxicity, B-cell aplasia | CRS (grade 1-2), infections | Hepatitis, colitis, endocrinopathies |
Key Eligibility Criteria
- Relapsed/refractory myeloma
- At least 3 prior lines
- ECOG ≤ 2
- Creatinine clearance > 30 ml/min
- Adequate marrow reserve
Side Effect Management
- Early grading using Lee criteria
- Supportive care (antipyretics, IV fluids)
- Targeted therapy (tocilizumab for CRS ≥2)
- Neurotoxicity monitoring with ICE score
- Prophylactic antivirals and immunoglobulin
Important Note
This tool provides educational information only. Always consult with your healthcare team about treatment options and eligibility for immunotherapy.
When you hear the phrase multiple myeloma immunotherapy, you might wonder how a blood‑cancer patient could benefit from a treatment that “hijacks” the immune system. In the past few years, scientists have turned the concept from theory into several FDA‑approved options that can produce deep, lasting responses for patients who have exhausted standard drugs.
What is Multiple Myeloma?
Multiple Myeloma is a cancer of plasma cells, the antibody‑producing factories in bone marrow. As malignant plasma cells multiply, they crowd out healthy blood cells, cause bone lesions, and release abnormal proteins that damage kidneys. According to the International Myeloma Working Group, about 35,000 new cases are diagnosed in the United States each year, and the median age at diagnosis is 70.
How Immunotherapy Works for Myeloma
Immunotherapy is a broad term for treatments that empower the body's own defenses to recognize and kill cancer cells. In myeloma, the goal is to expose unique markers on plasma cells-most notably B‑cell maturation antigen (BCMA)-and then direct immune effectors (T‑cells, antibodies, or engineered proteins) against them.
The three main strategies in current practice are CART‑cell therapy, bispecific antibodies, and checkpoint inhibitors. Each uses a different mechanism but shares the same principle: turn a weak immune response into a laser‑focused attack on myeloma cells.
Key Immunotherapy Modalities
Below is a quick look at the three FDA‑approved options as of 2024.
| Modality | Mechanism | FDA Approval Year | Typical Response Rate | Administration | Main Side Effects |
|---|---|---|---|---|---|
| CAR T‑cell therapy (e.g., ide‑cel, cil‑cel) | Patient’s T‑cells are engineered to express a receptor that binds BCMA on myeloma cells. | 2021 (ide‑cel), 2022 (cil‑cel) | ≈80% overall response, 40% complete remission | Single infusion after lymphodepletion (hospital stay 2‑3days) | Cytokine Release Syndrome, neurotoxicity, B‑cell aplasia |
| Bispecific Antibody (e.g., teclistamab) | Simultaneously binds BCMA on tumor cells and CD3 on T‑cells, forming a cytolytic bridge. | 2022 | ≈63% overall response, 40% complete remission | Weekly subcutaneous injection after step‑up dosing | Cytokine Release Syndrome (mostly grade1‑2), infections |
| Checkpoint Inhibitor (e.g., pembrolizumab off‑label) | Blocks PD‑1/PD‑L1 interaction, releasing T‑cell inhibition. | Not yet FDA‑approved for myeloma (clinical trials ongoing) | Modest activity as monotherapy; better in combination. | IV infusion every 3weeks | Immune‑related hepatitis, colitis, endocrinopathies |
Who Is a Good Candidate?
Eligibility depends on disease status, prior therapies, and overall health. Generally, these therapies are offered to patients with relapsed or refractory myeloma who have received at least three prior lines, including a proteasome inhibitor, an immunomodulatory drug, and an anti‑CD38 antibody.
Key factors doctors look at:
- Performance status (ECOG ≤2)
- Kidney function - creatinine clearance >30ml/min for most CART products
- Absence of uncontrolled infections
- Adequate marrow reserve - neutrophils >1,000/µL, platelets >50,000/µL
Patients with severe cardiac disease or active CNS involvement are usually excluded from CART trials, while bispecific antibodies can be used in a broader population because they don’t require cell manufacturing.
Managing Side Effects
Cytokine Release Syndrome (CRS) is the most common toxicity after CART or bispecific therapy. It ranges from mild fever to life‑threatening hypotension.
Management steps:
- Early grading using the Lee criteria. \n
- Supportive care - antipyretics, IV fluids.
- Targeted therapy - tocilizumab (IL‑6 blocker) for grade≥2, steroids for refractory cases.
Neurotoxicity (ICANS) occurs in about 30% of CART recipients. Monitoring with the ICE score and prompt steroids can prevent progression.
Long‑term immune suppression can lead to infections; prophylactic antivirals, antifungals, and immunoglobulin replacement are standard.
Future Directions
Research is already expanding beyond BCMA. New targets such as GPRC5D and FcRH5 are entering early‑phase trials, promising to overcome resistance when myeloma cells down‑regulate BCMA.
Combination strategies-pairing bispecific antibodies with IMiDs, or CART cells with checkpoint blockade-are showing deeper responses in pilot studies. Additionally, all‑ogeneic CART (off‑the‑shelf) aims to cut manufacturing time from weeks to hours.
Practical Checklist for Patients
- Ask about eligibility: "How many prior lines have I had, and do I meet the performance criteria?"
- Discuss logistics: manufacturing time for CART (typically 2‑3weeks), infusion center location, and insurance coverage.
- Plan for side‑effect monitoring: "Will I need an overnight stay for CRS observation?"
- Review supportive care: vaccines, infection prophylaxis, and blood product needs.
- Consider future options: if one immunotherapy fails, ask about alternative targets or clinical trial enrollment.

Frequently Asked Questions
What makes immunotherapy different from traditional chemotherapy?
Chemotherapy attacks any rapidly dividing cell, which causes broad toxicity. Immunotherapy aims at a specific cancer antigen-like BCMA-so it can spare most normal tissues and often produces deeper, longer responses.
Is CAR T‑cell therapy a cure for myeloma?
It’s not a guaranteed cure, but many patients achieve complete remission lasting several years-far longer than with older regimens. Ongoing monitoring is still essential.
How long does a bispecific antibody treatment last?
Patients usually stay on the drug until disease progression or unacceptable toxicity. Because the drug is given weekly, the treatment can continue for years if it stays effective.
Can I receive immunotherapy after a stem‑cell transplant?
Yes, many trials enroll patients who have already had an autologous transplant. The transplant can actually improve immune recovery before a CART infusion.
What role does the FDA play in these therapies?
FDA evaluates clinical trial data, assesses safety, and grants approval for each specific product and indication.






The landscape of myeloma treatment has been irrevocably altered by the advent of immunotherapy.
Where once clinicians relied solely on proteasome inhibitors and immunomodulatory drugs, now engineered cellular constructs and bispecific antibodies dominate the conversation.
CAR‑T cell therapy, exemplified by ide‑cel and cil‑cel, ushers in a paradigm wherein a patient's own T‑cells are harvested, genetically reprogrammed, and returned as living drugs.
The reported overall response rates approaching 80 percent, with complete remissions in roughly forty percent of heavily pre‑treated patients, are nothing short of revolutionary.
Yet these numbers belied a spectrum of toxicities that demand vigilant monitoring, most notably cytokine release syndrome and neurotoxicity, which can crescendo to life‑threatening levels if left unchecked.
Bispecific antibodies such as teclistamab, on the other hand, sidestep the logistical labyrinth of ex‑vivo cell manufacturing by acting as an off‑the‑shelf bridge linking BCMA on myeloma cells to CD3 on T‑cells.
Their weekly subcutaneous administration confers a convenience factor that is particularly appealing to patients reluctant to endure a hospital stay for a single infusion.
Though their overall response rates hover around sixty‑three percent, the safety profile appears more manageable, with most cytokine release events limited to grade one or two.
Checkpoint inhibitors, while still awaiting FDA endorsement for myeloma, represent a compelling avenue when combined with other immunotherapies, potentially ameliorating the immune exhaustion observed after repeated antigen exposure.
The biochemical underpinnings of this exhaustion involve upregulation of PD‑1 and CTLA‑4 pathways, which checkpoint blockade seeks to reverse.
Nevertheless, the modest monotherapy activity of agents like pembrolizumab underscores the necessity of rational combination strategies.
Emerging targets beyond BCMA-GPRC5D, FcRH5-promise to circumvent antigen escape, a phenomenon increasingly observed in relapsed cases.
All‑ogeneic CAR‑T cells, with their off‑the‑shelf availability, could truncate manufacturing timelines from weeks to mere hours, democratizing access for patients with rapid disease progression.
Concurrently, the integration of immunomodulatory drugs such as lenalidomide into bispecific regimens has demonstrated synergistic potency in early phase trials.
In sum, the myeloma immunotherapy arsenal is expanding at a breathtaking pace, demanding that both clinicians and patients remain abreast of evolving data to make informed therapeutic choices.
Great summary! 😊
The comparison table effectively distills complex mechanisms into an accessible format.
From a mechanistic standpoint, engineered T‑cells targeting BCMA represent a sophisticated form of precision medicine.
Moreover, the CRS incidence across CAR‑T and bispecifics underscores a shared immunologic challenge that necessitates vigilant prophylaxis.
It is noteworthy that checkpoint inhibitors, despite modest monotherapy activity, still hold promise in combinatorial regimens.
Overall, the data presented affirms the momentum of immunotherapy as a cornerstone in relapsed/refractory myeloma management.
Clinicians must, however, balance efficacy with the logistical demands of each modality to optimize patient outcomes.
While the efficacy figures are impressive, it's essential to remember the patient perspective in this evolving landscape.
The necessity for overnight monitoring after CAR‑T infusions can be a significant burden for those living far from specialized centers.
Bispecific antibodies, with their subcutaneous route, may alleviate some of this logistical strain, offering a more patient‑friendly schedule.
Nevertheless, each therapy's toxicity profile demands individualized counseling to ensure patients are fully informed about potential risks and benefits.
One might contemplate the philosophical shift from treating symptoms to re‑educating the immune system itself.
This transition mirrors a broader trend in medicine, where the focus moves from destructive interventions toward restorative approaches.
In the context of myeloma, harnessing endogenous cellular mechanisms may ultimately redefine what we consider curative.
Ever wonder why the big pharma giants are so eager to push CAR‑T while keeping the off‑the‑shelf versions under wraps?
It feels like there’s an entire hidden agenda to control the supply chain and keep the profits flowing.
Just a friendly reminder to stay skeptical and keep digging for the truth behind the headlines.
The prospect of all‑ogeneic CAR‑T cells is truly fascinating, as it could dramatically reduce manufacturing delays that currently limit access for patients with aggressive disease.
Furthermore, expanding the antigen repertoire beyond BCMA may help circumvent resistance mechanisms that arise from antigen loss.
I appreciate the thoroughness of this guide; it serves as a valuable resource for patients navigating complex treatment decisions.
It is especially helpful that side‑effect management strategies are clearly outlined, as proactive care can mitigate many of the severe toxicities associated with immunotherapy.
Please continue to update the community with emerging data as new trials progress.
For anyone considering CAR‑T or bispecific therapy, here are some practical tips: ensure baseline cardiac evaluation, maintain up‑to‑date vaccination status, and arrange a post‑infusion monitoring plan with your care team; prophylactic antivirals (e.g., acyclovir) and immunoglobulin replacement can significantly reduce infection risk; early recognition of CRS-characterized by fever, hypotension, hypoxia-allows for prompt tocilizumab administration; and finally, keep a detailed symptom diary to facilitate communication with clinicians during follow‑up.
The article commendably aggregates the current FDA‑approved immunotherapies, yet it glosses over the substantial heterogeneity in patient selection criteria across trials.
Such omissions risk oversimplifying the decision‑making process for clinicians who must reconcile individual comorbidities with therapeutic risk‑benefit profiles.
It would be prudent to include a more nuanced discussion of real‑world outcomes versus controlled trial data.