Gut Absorption Calculator
How Your Gut Affects Medication
This tool estimates how much of your oral medication might be absorbed based on key factors from the article. Results are approximate and should not replace medical advice.
Estimated Absorption
Factors affecting absorption:
- Severe disease may reduce absorption by 40-60%
- High-fat meals can decrease peak levels by 30-50%
- Medication type significantly impacts absorption
Take a pill. It seems simple. But inside your body, that pill faces a battlefield. The stomach churns, the intestines move, enzymes break things down, and your body’s natural defenses work hard to keep foreign substances out. For many gastrointestinal medications, this isn’t just a minor inconvenience-it’s the reason they don’t work as well as they should.
Why Your Pill Might Not Be Working
Most drugs you take by mouth are meant to be absorbed through the walls of your small intestine. That’s where the real action happens. The small intestine has a surface area roughly the size of a tennis court, thanks to tiny finger-like projections called villi and microvilli. But even with all that space, absorption isn’t guaranteed. Many drugs simply can’t get through. Drugs need to be small and fat-soluble to slip easily across the intestinal lining. If a drug is too large-over 500 daltons-or too water-soluble, it gets stuck. Insulin, for example, has a molecular weight of nearly 6,000. Without special delivery systems, less than 1% of an oral dose ever reaches your bloodstream. That’s why insulin is still injected. Even when a drug is the right size, other barriers get in the way. The mucus layer lining your gut can trap pills before they dissolve. Enzymes in your gut and liver can break them down before they even get started. And then there’s P-glycoprotein-a kind of bouncer on your intestinal cells that kicks out drugs it doesn’t like. Many antibiotics, blood thinners, and even some cancer drugs are targets.Food, pH, and Timing: The Hidden Variables
You’ve probably been told to take some meds on an empty stomach. There’s a reason. Food doesn’t just fill your belly-it changes how your body handles drugs. Fatty meals can slow down how fast your stomach empties by 2 to 4 hours. That delay can cut peak blood levels of certain drugs by 30 to 50%. Levothyroxine, used for thyroid problems, is a classic example. If you take it with coffee, calcium, or breakfast, your body absorbs much less of it. The result? Your thyroid levels stay off, and you keep feeling tired. The pH of your gut also shifts along its length. Your stomach is acidic (pH 1-3), but by the time you reach the lower small intestine, it’s nearly neutral (pH 7-8). Some drugs dissolve better in acid, others in alkaline environments. If a drug isn’t designed to release in the right spot, it won’t absorb properly. That’s why some pills have coatings that only dissolve in the intestine-not the stomach.Disease Changes Everything
If you have Crohn’s disease, ulcerative colitis, or short bowel syndrome, your gut isn’t working the way it should. And that changes how drugs behave. In ulcerative colitis, inflammation can damage the intestinal lining. Studies show patients absorb 25-40% less of certain drugs like mesalamine compared to healthy people. One patient on a Crohn’s forum shared that their Remicade levels kept fluctuating-even with perfect dosing. That’s not noncompliance. That’s the disease messing with absorption. Short bowel syndrome is even more extreme. With less intestine to absorb drugs, patients often need 2-3 times the normal dose of antibiotics, vitamins, or pain meds just to get the same effect. And even then, it’s hit or miss. Then there’s the impact of other medications. GLP-1 receptor agonists like semaglutide (used for diabetes and weight loss) slow down gut movement. That’s good for blood sugar control-but bad if you’re also taking a blood thinner like warfarin. One pharmacist reported INR levels swinging from 1.5 to 4.5 in IBD patients on warfarin, even when the dose stayed the same. That’s a dangerous gap between under-dosing and over-dosing.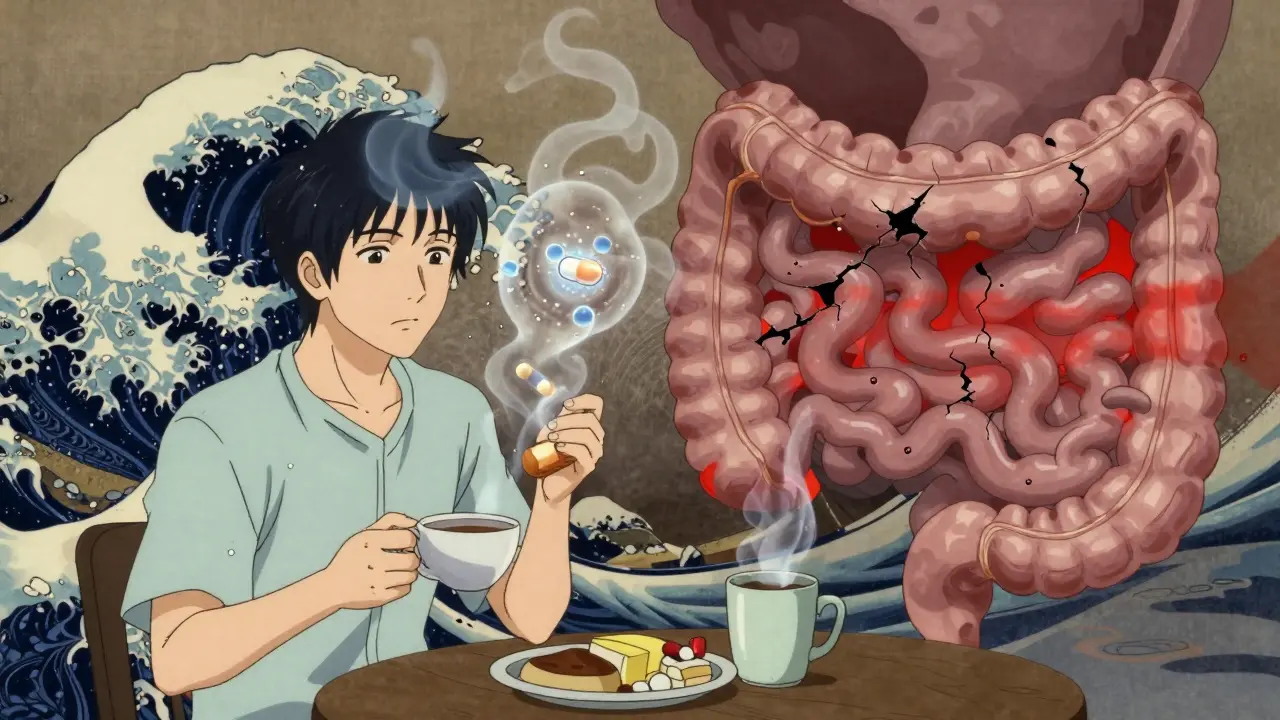
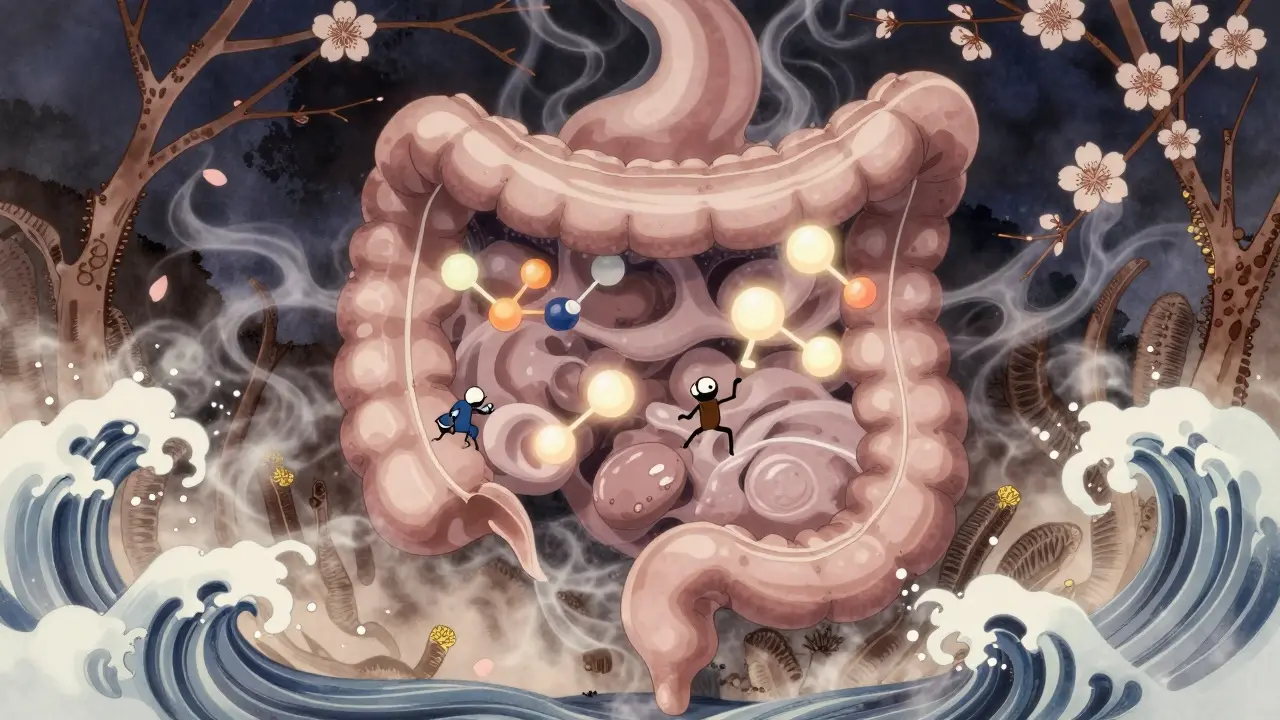
Formulation Matters More Than You Think
Not all pills are created equal. Two brands of the same drug can behave completely differently in your body. A tablet might dissolve too slowly. A capsule might not break open in the right section of your gut. Drug manufacturers can tweak the formulation-changing the salt form, crystal structure, or adding special coatings-to make absorption faster or slower. For example, switching from a regular tablet to a soluble salt form can boost absorption by 2 to 5 times. Newer approaches are getting smarter. Liposomes, nanoparticles, and lipid-based carriers can help drugs sneak through the gut wall. Some additives, like sodium caprate or chitosan, can temporarily open the tight junctions between cells, letting more drug through. These aren’t magic tricks-they’re science. And they’re already being used in newer formulations. But here’s the problem: most drug labels don’t tell you which formulations work best for people with gut diseases. Only 15-20% of oral medications have specific guidance for IBD patients. That means doctors and pharmacists are often guessing.What You Can Do
If you’re taking oral meds and they don’t seem to be working:- Take them exactly as directed. Empty stomach? Don’t eat for an hour before and after. No coffee, dairy, or antacids.
- Ask about formulation. Is there a liquid, chewable, or extended-release version? Some forms absorb better in certain conditions.
- Track your symptoms and blood levels. If you’re on warfarin, thyroid meds, or immunosuppressants, regular lab tests can show if absorption is the issue.
- Speak to a clinical pharmacist. They specialize in how drugs behave in the body. A 6-12 month training program exists just for this.

The Future: Personalized Gut Medicine
Scientists are now building digital models of the gut that simulate how drugs behave in people with Crohn’s, IBS, or after bowel resection. These models are 85-90% accurate in predicting real-world outcomes. Some startups are testing smart capsules with sensors that measure pH, pressure, and transit time as they move through your gut. The data could one day tell your doctor: “Your absorption of this drug is 40% lower than normal-try this dose instead.” Meanwhile, the market for absorption enhancers is set to hit $2.8 billion by 2027. Big pharma is finally investing in this. Why? Because 70% of new drugs in late-stage trials are too big or too water-soluble to absorb well. If we can’t fix absorption, we can’t deliver the next generation of medicines.Bottom Line
Your gut isn’t just a tube for food. It’s a complex, dynamic filter for drugs. What works for one person might fail for another-not because they’re not following instructions, but because their gut is different. If you’ve ever wondered why your medication doesn’t seem to work like it should, the answer might be hiding in your intestines-not your adherence.Why do some GI medications work for some people but not others?
Differences in gut health, disease severity, transit time, pH levels, and even genetics affect how drugs are absorbed. Two people with the same diagnosis can have wildly different absorption rates. For example, someone with mild ulcerative colitis might absorb 80% of a dose, while someone with severe inflammation may absorb only 50%. Formulation, food timing, and other medications also play a role.
Can food really make a difference in how well my pills work?
Yes. Fatty meals can delay stomach emptying by 2-4 hours, reducing peak drug levels by 30-50%. Levothyroxine, antibiotics like tetracycline, and some antifungals are especially sensitive. Even coffee, calcium supplements, or iron can bind to drugs and block absorption. Always follow dosing instructions about food.
Why do some pills have special coatings?
Coatings protect drugs from stomach acid or delay release until they reach the small intestine. For example, delayed-release mesalamine avoids breaking down in the stomach so it can target the colon. Other coatings dissolve only at specific pH levels-like those used in enteric-coated aspirin to prevent stomach irritation.
Are liquid or chewable forms better for absorption?
For children, elderly, or people with swallowing issues, yes. Liquids and chewables often dissolve faster than tablets, leading to quicker absorption. But for drugs that need to be released in a specific part of the gut-like colon-targeted meds-formulation matters more than physical form. Always check with your pharmacist.
What should I do if my medication doesn’t seem to be working?
Don’t just increase the dose. Talk to your doctor or a clinical pharmacist. Ask for blood level testing if possible (e.g., INR for warfarin, TSH for thyroid meds). Check if your condition has changed (like new inflammation or surgery). Ask if a different formulation exists. Sometimes, switching brands or forms can make all the difference.



This is so real. I’ve been on mesalamine for years and my doctor kept saying I wasn’t compliant until I got my blood levels checked-turns out my inflammation was eating up half the dose. Finally switched to a different formulation and life changed.
Thank you for writing this.
Oh wow. So the reason my warfarin’s been a nightmare isn’t because I’m a terrible patient but because my gut is just… uncooperative? Shocking. I thought I was the problem. Turns out my intestines are just really bad at their job.
YES. I’ve been telling my GI doc for months that my meds ‘don’t work’ and they kept blaming me. Then I found out my Crohn’s flares were literally blocking absorption. I’m now on a liquid version of my immunosuppressant and my levels are stable for the first time in 3 years. 🙌
Let’s be honest here-this isn’t just about pills and pH levels. This is about the entire pharmaceutical industry’s refusal to acknowledge that human biology isn’t a factory line. We’re not widgets. We’re not even standardized test subjects. We’re messy, dynamic, emotionally and physiologically complex organisms with trillions of microbes, fluctuating enzyme levels, and gut motility that changes based on stress, sleep, and whether we had a bad breakup last night.
And yet, we’re told to take a pill at 8 AM, no food, no coffee, no distractions, like we’re robots programmed by a corporate algorithm. The fact that 70% of new drugs fail because they can’t be absorbed? That’s not a scientific problem. That’s a philosophical failure. We’re treating biology like it’s a software bug to be patched, not a living ecosystem to be understood. And until we stop pretending that one-size-fits-all dosing works for everyone, we’re just throwing money at the problem while real people suffer in silence.
Also, sodium caprate? That’s wild. It’s basically a molecular crowbar. Imagine if we could just open up the tight junctions like a garage door for drugs. We’re not far from sci-fi anymore. The gut isn’t a pipe. It’s a sentient, adaptive, deeply personal interface between the outside world and your internal universe. And we’re still treating it like a vending machine.
TL;DR: Gut = filter. Drug = intruder. P-gp = bouncer. Food = distraction. Inflammation = broken lock. Pharma = lazy. Formulation = afterthought. Dose = guesswork. You’re not noncompliant. Your gut is just broken in ways we don’t measure.
My doctor told me to take my thyroid med on an empty stomach. I did. Still felt like a zombie. Turns out my coffee was binding it. No one told me that. Now I wait 90 minutes. Life’s better. But why is this info so hard to find?
Look I’ve read a lot of this stuff and I think most people just dont get it. The body is a complex system and you cant just shove a pill in and expect it to work like magic. I mean cmon. The liver breaks down half of everything and the gut is like a maze with guards and traps. And dont even get me started on how some people have like 30% of their intestine gone and still expect the same dose to work. Its insane. The system is broken. Pharma cares more about patenting new salts than making sure people actually absorb the damn thing. And doctors? They just prescribe and hope. Thats not medicine thats gambling.
As someone from India with IBS, I’ve had to try 5 different brands of my acid reflux meds before one actually worked. Turns out the coating dissolved too fast in my fast-moving gut. No one told me to ask about formulation. Just switched brands and boom-no more burning. 🙏
My cousin in Nigeria takes antibiotics for malaria and they don’t work half the time. We thought it was fake meds. Turns out his gut is full of parasites and the drugs just get trapped. No one in his village knows this. This post should be translated into 10 languages.
So let me get this straight-if you have Crohn’s, your body might only absorb 50% of your meds, but you’re still charged full price? And your doctor doesn’t adjust the dose because the label doesn’t say to? That’s not just flawed. That’s unethical.
Why isn’t there a database for drug absorption rates by condition? Why are we still flying blind? I get that science is hard, but if 70% of new drugs fail because of absorption, shouldn’t that be the #1 R&D priority? Not marketing.
As a clinical pharmacist, I’ve seen this daily. A patient on cyclosporine with ulcerative colitis? Absorption drops 40%. We double the dose. Still low. We switch to a different salt form-levels normalize. No one told them the brand mattered. The label doesn’t say. The doctor assumes compliance. The patient assumes the drug is broken. It’s a perfect storm of misinformation.
Ask for therapeutic drug monitoring. It’s not expensive. It’s life-changing.
This makes sense. My dad had part of his intestine removed. He takes 3x the dose of his vitamins and still gets weak. We thought he was just old. Turns out his gut just doesn’t hold on to stuff. This post helped me understand why. Thank you.