DOAC vs Warfarin Selection Tool
This tool helps you understand whether DOACs (apixaban, rivaroxaban, dabigatran, edoxaban) or warfarin might be more appropriate for your condition based on your specific health factors. All recommendations follow the latest clinical guidelines presented in the article.
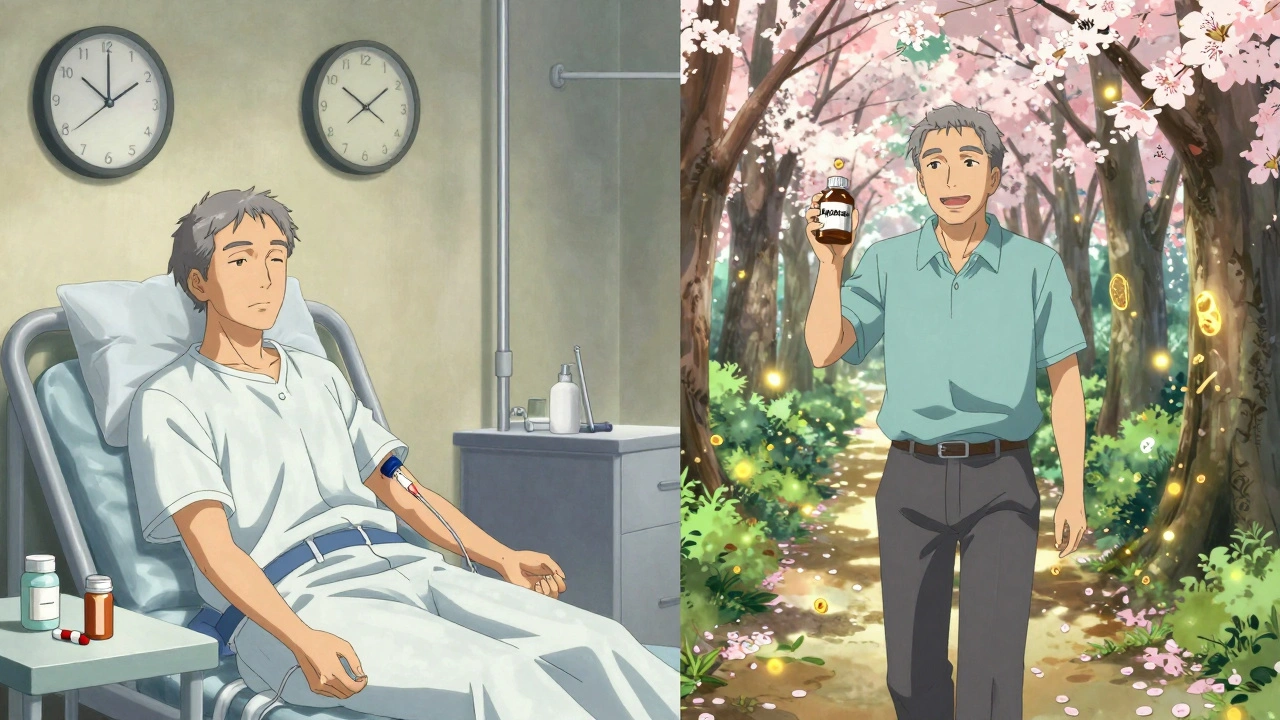
Choosing a blood thinner isn’t just about stopping clots-it’s about living without constant worry. For millions of people with atrial fibrillation, deep vein thrombosis, or pulmonary embolism, the choice between DOACs and warfarin comes down to one thing: which one lets you live better, with fewer surprises.
What You’re Really Choosing
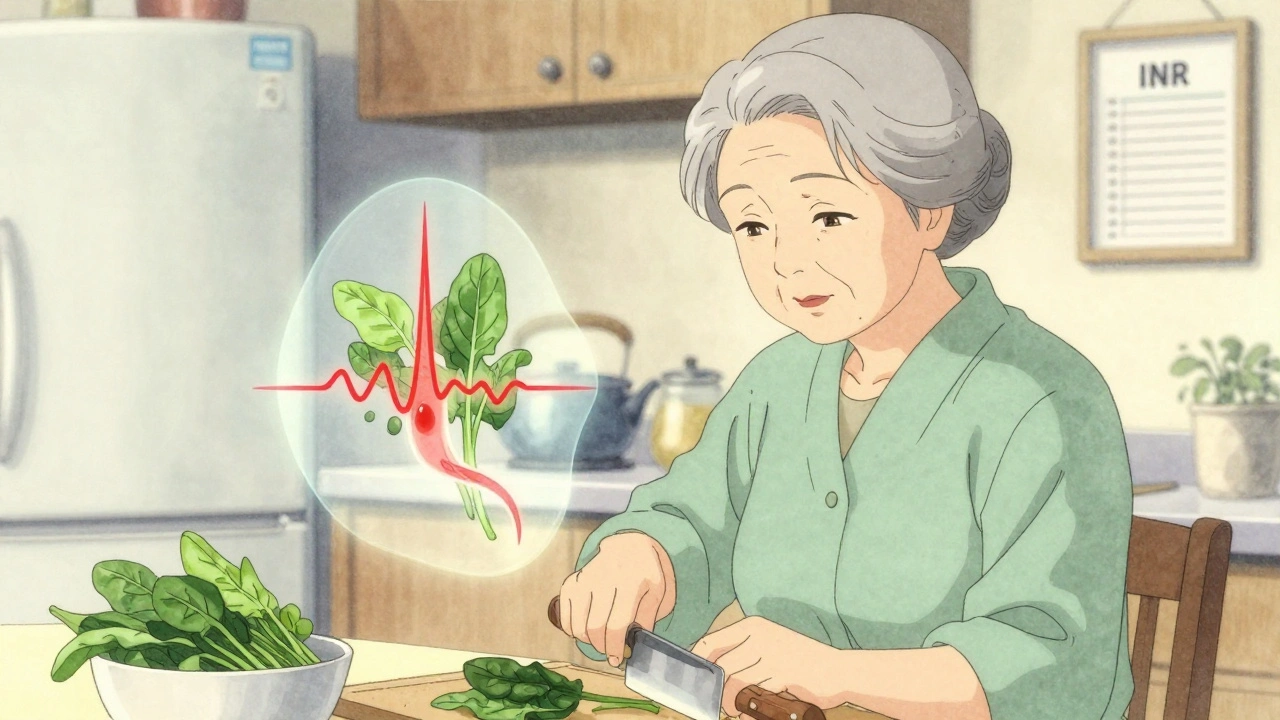
Warfarin has been around since the 1950s. It’s cheap. It’s well-known. But it’s also finicky. You need blood tests every week or two. Your diet matters-spinach, kale, broccoli can throw your INR off. Even a new antibiotic or over-the-counter painkiller can send your numbers flying. One patient in Adelaide told me she spent her first year on warfarin terrified to eat salad, afraid her INR would crash. DOACs-apixaban, rivaroxaban, dabigatran, edoxaban-are the new kids on the block. They don’t need weekly blood tests. You take the same dose every day. No dietary restrictions. Fewer drug interactions. That’s the promise. But are they safer? And if so, how much safer?Bleeding Risks: The Real Difference
The biggest advantage of DOACs isn’t convenience-it’s safety. Specifically, fewer life-threatening bleeds. A 2024 meta-analysis of over 100,000 patients found DOACs reduced major bleeding by 30% compared to warfarin. That’s not a small number. It means for every 100 people switching from warfarin to a DOAC, about 3 major bleeds are avoided each year. The biggest drop? In brain bleeds. Warfarin carries a 50-60% higher risk of intracranial hemorrhage than DOACs. That’s the kind of bleed that can kill or leave you permanently disabled. Apixaban, in particular, shows the lowest bleeding rate among DOACs-just 1.9 events per 100 person-years, compared to 2.4 for warfarin and 2.8 for rivaroxaban. But here’s the catch: not all DOACs are the same. Rivaroxaban has a higher risk of stomach bleeding than apixaban. If you’ve had a GI bleed before, apixaban is the clear pick. Dabigatran carries a slightly higher risk of gastrointestinal bleeding than other DOACs, especially in older adults. Warfarin’s bleeding risk isn’t just about the drug-it’s about how well your INR is controlled. If your time in therapeutic range (TTR) is below 60%, your bleeding risk jumps to match or even exceed DOAC levels. Many clinics in rural areas or under-resourced hospitals struggle to keep TTR above 65%. In those cases, DOACs aren’t just better-they’re safer by default.When Warfarin Still Wins
DOACs aren’t perfect for everyone. There are three clear situations where warfarin is still the only option:- People with mechanical heart valves-DOACs can cause deadly clots here. Warfarin is mandatory.
- Patients with antiphospholipid syndrome-those with repeated clots and specific antibodies. DOACs increase their risk of clots by nearly three times compared to warfarin.
- Severe kidney failure (CrCl under 15-30 mL/min). Most DOACs aren’t cleared properly in these patients. Warfarin, though harder to manage, remains the only option.
Cost: The Hidden Barrier
Warfarin costs $4 to $10 a month. DOACs? $450 to $600 without insurance. That’s a huge gap. But here’s what most people don’t realize: the real cost of warfarin isn’t the pill. It’s the blood tests. The clinic visits. The time off work. The emergency room trips when your INR spikes. A 2024 study found warfarin becomes more expensive than DOACs after just 13 INR tests per year. For many patients, that happens in three months. Most Medicare Part D and private insurers now cover DOACs at a $30-$100 copay. That makes them affordable for most. But for those without insurance-especially in Australia, where PBS subsidies don’t cover all DOACs for all indications-the cost can be a dealbreaker. One Reddit user from Perth wrote: “I’m on warfarin because I can’t afford Eliquis. My INR is always weird, but at least I’m not choosing between medicine and groceries.”Convenience Isn’t Just a Bonus-It’s a Lifesaver
A 2023 survey of 1,247 anticoagulant users found 78% of DOAC users said their quality of life improved. Only 42% of warfarin users said the same. Why? Three reasons:- 89% of DOAC users didn’t have to change their diet.
- 85% didn’t need regular blood draws.
- 71% of warfarin users reported unpredictable INR swings-sometimes without any obvious cause.

What Doctors Actually Recommend
Guidelines from the American Heart Association, American College of Cardiology, and CHEST all strongly favor DOACs for non-valvular atrial fibrillation and most cases of VTE. The strongest recommendation? Apixaban. Why apixaban? It’s the safest. It’s the most forgiving. It works well in older patients, in those with low body weight, and in people with mild kidney issues. The 2024 JACC study found apixaban had the lowest bleeding rate of any anticoagulant-lower than warfarin, lower than other DOACs. Doctors now use a simple 5-point scoring system to pick the right drug:- Age over 75
- Reduced kidney function
- History of bleeding
- Taking aspirin or other blood thinners
- Female sex
What Can Go Wrong?
DOACs aren’t risk-free. The biggest mistake? Dosing errors in people with kidney problems. Eighteen percent of patients on DOACs get the wrong dose because their creatinine clearance wasn’t checked properly. That can lead to overdose and bleeding. Another issue: combining DOACs with NSAIDs like ibuprofen or naproxen. The FDA issued a warning in January 2024: using NSAIDs with DOACs doubles the risk of stomach bleeding. Acetaminophen (paracetamol) is safer. And yes-DOACs can’t be reversed as easily as warfarin. But that’s changing. Idarucizumab reverses dabigatran. Andexanet alfa reverses apixaban and rivaroxaban. These drugs are in most hospitals now. Warfarin can be reversed with vitamin K or clotting factors, but it takes hours. DOAC reversal can happen in minutes.What Should You Do?
If you’re on warfarin and doing fine-stable INR, no bleeds, no dietary stress-there’s no need to switch. But if you’re struggling with frequent tests, diet restrictions, or unpredictable results, talk to your doctor about DOACs. If you’re starting anticoagulation for the first time, DOACs should be your first option-unless you have a mechanical valve, antiphospholipid syndrome, or severe kidney disease. Ask your doctor:- Which DOAC is best for my age, kidney function, and bleeding risk?
- Is apixaban an option? It’s the safest.
- Can we check my kidney function before starting?
- What if I miss a dose?
- What painkillers are safe to take with this?
Are DOACs safer than warfarin?
Yes, overall. DOACs reduce the risk of major bleeding by about 30% compared to warfarin, especially dangerous brain bleeds. Apixaban has the lowest bleeding risk among DOACs. However, they’re not safer for everyone-people with mechanical heart valves or antiphospholipid syndrome still need warfarin.
Can I switch from warfarin to a DOAC?
Most people can, but it must be done under medical supervision. Your doctor will check your kidney function, current INR, and any other medications you’re taking. Switching is usually safe if you don’t have a mechanical valve, severe kidney disease, or antiphospholipid syndrome.
Why is apixaban recommended over other DOACs?
Apixaban has the lowest rate of major bleeding in clinical trials-1.9 events per 100 person-years, compared to 2.4 for warfarin and up to 2.8 for rivaroxaban. It’s also more forgiving in older adults, people with low body weight, and those with mild kidney issues. Guidelines now recommend it as the first-choice DOAC for most patients.
Do I need blood tests with DOACs?
No routine blood tests are needed for DOACs. However, your doctor will check your kidney function (creatinine clearance) every 6 to 12 months, especially if you’re over 75 or have other health issues. This helps ensure you’re on the right dose.
What if I can’t afford DOACs?
Warfarin is much cheaper-just $4-$10 a month. If cost is a barrier, warfarin is still a valid option if you can manage regular INR tests and dietary consistency. Some pharmaceutical assistance programs or PBS subsidies may help reduce DOAC costs. Ask your pharmacist or doctor about options.
Can I take NSAIDs like ibuprofen with DOACs?
No. The FDA warns that combining NSAIDs (ibuprofen, naproxen) with DOACs increases the risk of stomach bleeding by more than double. Use acetaminophen (paracetamol) instead for pain relief. Always check with your doctor before taking any new medication.





I switched from warfarin to apixaban last year and honestly? I ate a whole damn kale salad last week and didn't check my INR. I cried. Not because I was scared-because I finally felt normal again.
Also, my dog now gets to sleep on the bed. Turns out, not having to plan your life around a blood test is the real luxury.
Guys, let me tell you something about DOACs-I read the entire JACC meta-analysis last night and let me just say, the 30% reduction in major bleeding is statistically significant but clinically overstated because the studies were mostly conducted in Western populations with access to good labs and nutrition. In India, where people eat high-vitamin K diets and skip doses because they can't afford follow-ups, the real-world benefit is way lower. Also, apixaban? It's expensive. Like, 'sell-a-kidney' expensive. We need cheaper generics. Also, did you know rivaroxaban has a higher GI bleed risk? I'm not just saying that-I'm a med student. I know.
I get that DOACs are better for most people, but let’s not forget warfarin saved lives for decades before all this fancy stuff came along. My uncle was on warfarin for 12 years-no issues, stable INR, loved his spinach. The key isn’t the drug-it’s the support system. If your clinic is good, your doctor listens, and you’ve got someone to remind you to take your pill? Warfarin still works. We don’t need to throw out the old just because the new is shinier.
Also, if you’re struggling with cost, talk to your pharmacist. There are programs. You’re not alone.
The entire discourse around DOACs is a neoliberal fantasy disguised as medical progress. We have commodified anticoagulation into a consumer choice-apixaban as the ‘premium’ option, warfarin as the ‘budget’ one-as if life-and-death decisions should be filtered through a CVS pharmacy loyalty program.
And yet, we ignore the structural violence: a woman in rural Kentucky can’t afford a $100 copay, so she risks intracranial hemorrhage not because of biology, but because capitalism prioritizes profit over personhood. Apixaban isn’t safer-it’s just more profitable.
Let me be clear: anyone who says DOACs are ‘better’ without mentioning the reversal agents is either lying or dangerously uninformed. Warfarin has been reversed for 60 years with vitamin K and fresh frozen plasma. DOACs? You need a $30,000 drug that only major hospitals stock.
And don’t even get me started on the ‘no blood tests’ myth. You still need kidney checks. You still need to monitor for bleeding. You still need to know what happens if you vomit after taking it.
This isn’t progress. It’s marketing dressed in white coats.
I’ve been on rivaroxaban for 3 years. I’ve had zero bleeds, zero blood tests, and I still eat tacos every Friday. But my doctor didn’t even check my creatinine until year two. That’s not ‘convenient’-that’s negligence.
Also, why is everyone acting like apixaban is some magic bullet? I know a guy who had a GI bleed on apixaban because he was on aspirin too. No one told him. So don’t just take the hype. Ask your doctor the hard questions.
From a clinical standpoint, the data is robust: DOACs reduce major bleeding by 30%, intracranial hemorrhage by 50-60%, and improve adherence by 10%+. Apixaban’s pharmacokinetics make it uniquely forgiving in elderly populations with fluctuating renal function. However, the real-world efficacy hinges on patient education. Many patients don’t realize that missing a DOAC dose isn’t harmless-especially if they’re on concomitant NSAIDs or have CKD.
Key takeaway: DOACs are superior for most, but only if dosing is appropriate and drug interactions are actively managed. Routine CrCl monitoring every 6-12 months is non-negotiable.
I don’t get why everyone’s acting like this is a new revelation. I’ve been on warfarin since 2018. My INR’s been stable for years. I eat my greens. I take my pill. I don’t need a fancy drug to live my life. This whole post feels like a pharma ad.
OMG I JUST SWITCHED TO APIXABAN AND I CAN EAT SALAD AGAIN 😭 I literally cried when my nurse said I didn’t need a blood test next week. I’ve been avoiding broccoli since 2020. Now I’m planning a trip to Italy. No more ‘I can’t go out of state because I need my INR checked’.
Also, my mom’s on warfarin and she’s terrified of her own shadow. She thinks if she sneezes wrong, she’ll bleed out. I’m so glad she’s gonna switch soon. You’re not broken if you need a better drug. You’re just human.
I don’t care how many studies say DOACs are safer. I’m American. I know how this works. Big Pharma pushes expensive drugs because they make more money. Warfarin is cheap because it’s old. That’s it. Don’t pretend this is about patient care. It’s about stock prices.
The notion that DOACs represent ‘freedom’ is a bourgeois fantasy. In Australia, PBS subsidies are conditional, and many patients are forced into warfarin not by clinical need, but by bureaucratic inertia. The ‘convenience’ of DOACs is a luxury only accessible to those who can navigate insurance labyrinths.
Meanwhile, the elderly, the undocumented, and the underinsured are left with outdated protocols-and then blamed for poor outcomes. This isn’t innovation. It’s exclusion dressed in clinical jargon. 🤷♂️
I had a stroke in 2021. They put me on warfarin. I was terrified. I didn’t leave the house for six months. Then I switched to apixaban. I went to a concert last month. I danced. I didn’t think I’d ever do that again.
This isn’t just about blood tests. It’s about getting your life back. I’m not saying everyone should switch. But if you’re scared, if you’re tired, if you’re tired of being a statistic-talk to your doctor. You deserve to breathe.
The cultural implications of anticoagulant choice are profound. Warfarin, with its rigid rituals of monitoring and dietary restriction, reinforces a medical model of control and compliance. DOACs, by contrast, embody a shift toward patient autonomy, temporal flexibility, and bodily liberation.
One need not be a bioethicist to recognize that the ability to eat a salad without fear is not trivial-it is existential. The pharmacological revolution here is not merely therapeutic, but ontological.
Apixaban is the best but only if your kidneys are good and you dont take ibuprofen and dont have mechanical valve or APS and you can afford it and your doctor checks your creatinine every 6 months and you dont have liver disease and you dont have history of GI bleed and you dont take St Johns wort and you dont have cancer and you dont have history of falls and you dont drink alcohol and you dont have atrial fibrillation with valve disease and you dont have any other meds and you dont have any other health issues and you dont have any other problems and you dont have any other anything
I’ve been on warfarin for 15 years. My INR is perfect. I know exactly how much kale I can eat. I know which antibiotics to avoid. I’ve had no bleeds. No emergencies. No stress.
So why are you telling me I need to switch? I’m not broken. I’m not failing. I’m just… doing fine.