BAS Medication Timing Calculator
This tool helps you calculate the minimum time separation needed between bile acid sequestrants (like cholestyramine, colestipol, or colesevelam) and other medications to avoid dangerous absorption issues.
Your Bile Acid Sequestrant
Add Your Other Medications
Your Medication Schedule
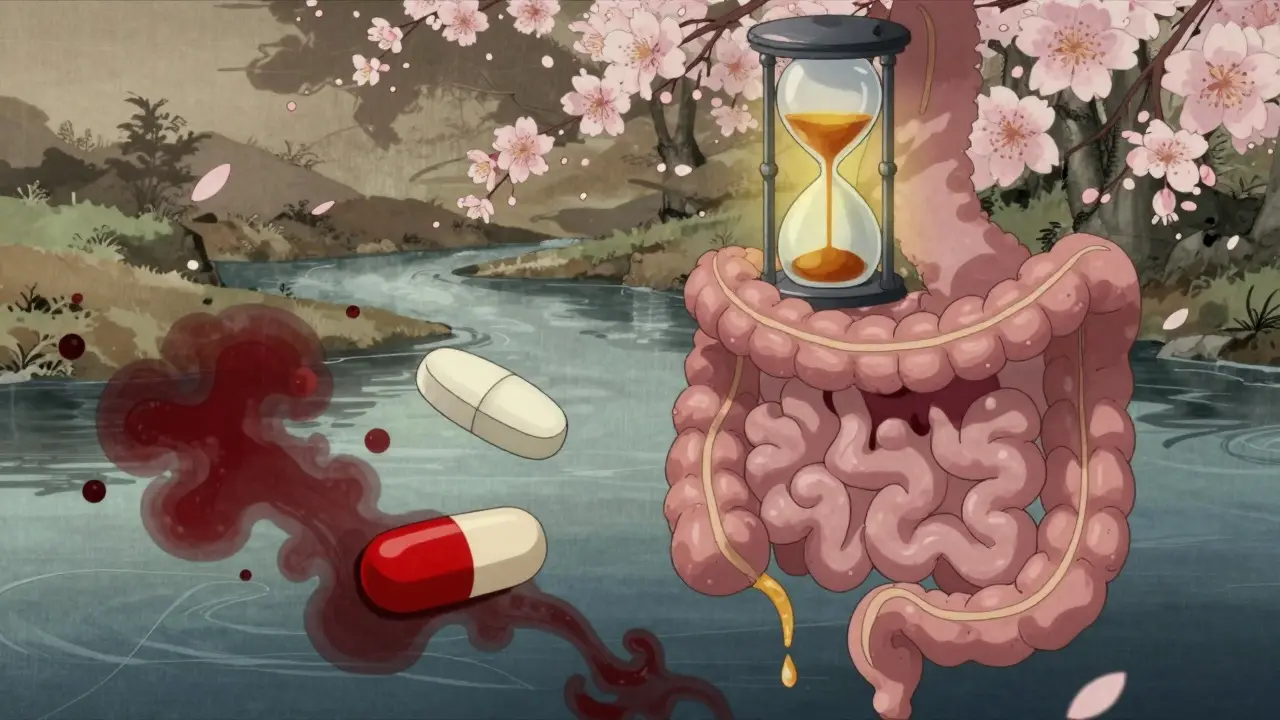
When you’re taking bile acid sequestrants like cholestyramine, colestipol, or colesevelam to lower your LDL cholesterol, you’re not just managing your heart health-you’re managing a complex schedule. These medications work by binding bile acids in your gut, which forces your liver to pull more cholesterol from your blood. Sounds simple, right? But here’s the catch: they don’t just bind bile acids. They bind medications, too. And if you don’t time things right, your other pills might just disappear before they ever get absorbed.
What Are Bile Acid Sequestrants and How Do They Work?
Bile acid sequestrants (BAS) are old-school cholesterol drugs that haven’t gone away for good reason. They’re not absorbed into your bloodstream. Instead, they sit in your intestines like sticky sponges, grabbing bile acids and flushing them out with your stool. Your liver notices the loss and starts pulling cholesterol from your blood to make more bile. That’s how your LDL drops-by 15% to 30%.
There are three main ones: cholestyramine (Questran), colestipol (Colestid), and colesevelam (Welchol). The first two come as powders you mix with water or juice. Colesevelam is a tablet, which is easier for many people. But all three share the same problem: they bind to other drugs.
Cholestyramine has the strongest binding power-about 3.5 mEq per gram. Colesevelam is a bit weaker at 2.8 mEq/g, which is why it causes fewer interactions. But even the weaker ones can mess with your meds if you don’t pay attention.
Why Timing Matters More Than You Think
Imagine taking your blood pressure pill, then swallowing your cholestyramine powder 30 minutes later. That blood pressure pill might get stuck to the resin in your gut and never make it into your bloodstream. Your blood pressure spikes. You feel dizzy. You think the medicine isn’t working. But it’s not the medicine-it’s the timing.
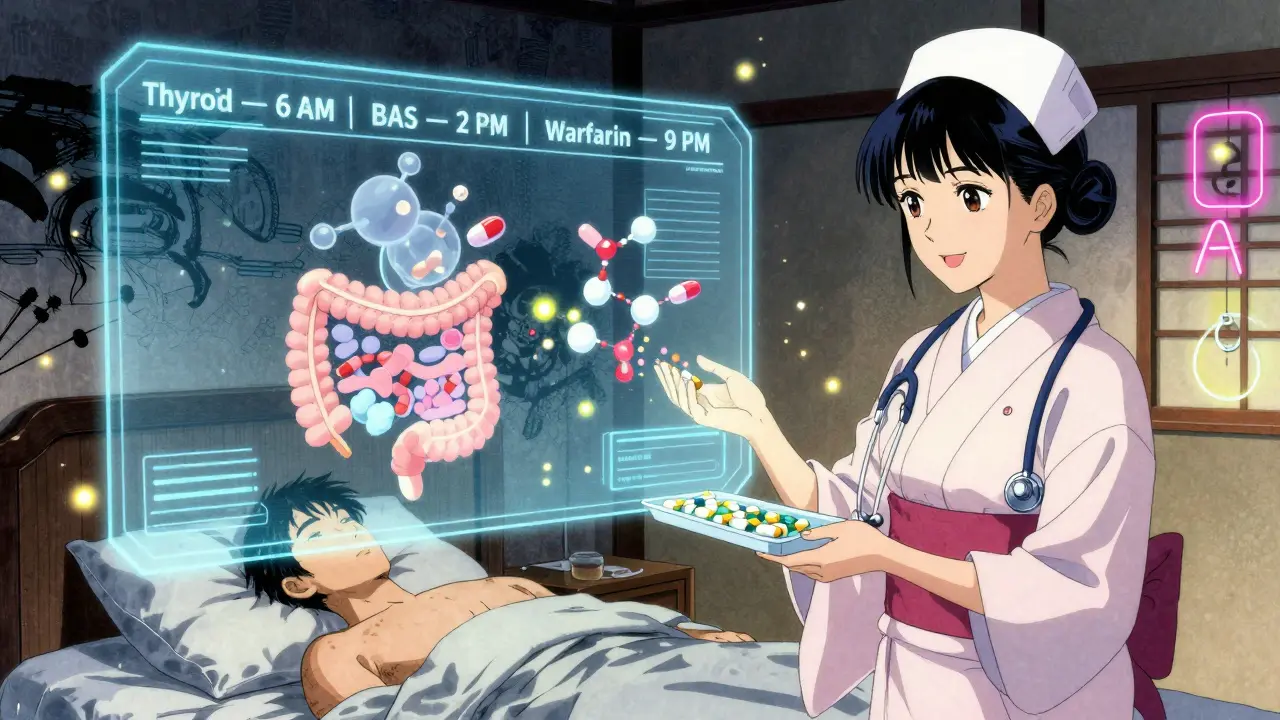
Studies show that when BAS are taken too close to other medications, absorption can drop by up to 50%. This isn’t theoretical. Real patients have had dangerous drops in INR (a measure of blood thinning) because warfarin didn’t get absorbed. Others have had thyroid levels crash because their levothyroxine was bound up.
Experts agree: you need to separate BAS from other medications by at least 4 hours. That’s the standard rule from the American College of Cardiology and the FDA labeling for cholestyramine. But here’s where it gets messy: some drugs need even more time.
Which Medications Are Most at Risk?
Not all drugs are affected the same way. Some are more vulnerable because they’re absorbed early in the gut, or because even a small drop in levels can be dangerous. Here’s what you need to watch for:
- Warfarin: Even a 4-hour gap might not be enough. Some studies show INR levels drop significantly if warfarin is taken within 6 hours of BAS. The safest bet? Take warfarin at least 6 hours before or after your BAS dose.
- Levothyroxine: This thyroid hormone is absorbed in the upper small intestine-right where BAS are most active. A 2022 study found that 23% of patients still had reduced absorption even with a 4-hour gap. For safety, aim for 8 hours between levothyroxine and BAS. Many doctors recommend taking levothyroxine first thing in the morning on an empty stomach, then waiting until after lunch to take BAS.
- Oral contraceptives: If your birth control pill doesn’t get absorbed, you’re not protected. There are documented cases of unintended pregnancy because the pill was bound by cholestyramine. Separate by at least 4 hours, and consider backup contraception if you’re inconsistent.
- Metformin: The extended-release version of metformin needs a 4-hour gap from colesevelam. Immediate-release metformin is less affected, but still best taken separately.
- Vitamins A, D, E, K: These fat-soluble vitamins get trapped along with bile acids. Long-term BAS users often need supplements. A 2019 study found 12.7% of users developed vitamin K deficiency, which can lead to abnormal bleeding.
- Antibiotics like tetracycline or fluoroquinolones: These can bind tightly to BAS. If you’re on antibiotics, delay your BAS dose until after the course ends, or separate by 6 hours.
Colesevelam vs. Cholestyramine: Which Is Easier to Manage?
If you’re starting BAS or switching, colesevelam (Welchol) is often the better choice-not because it’s stronger, but because it’s less messy. It doesn’t bind as tightly as cholestyramine, and it’s a tablet, not a chalky powder you have to mix.
Studies show colesevelam causes 30-40% fewer interactions with warfarin than cholestyramine. One user on EverydayHealth wrote: "I only need to separate my metformin by 2 hours with Welchol versus 4 hours with Questran, which fits better with my schedule." That’s not just anecdotal. Clinical trials back it up.
Cholestyramine, on the other hand, is cheaper (it’s generic), but harder to live with. It causes constipation in 57% of users, according to a 2023 study. That makes timing even harder-because if you’re bloated and stuck on the toilet, you’re less likely to stick to a strict schedule.
Real-Life Challenges: What Patients Actually Struggle With
It’s not enough to know the rules. You have to live them.
A 2022 survey of 452 BAS users found that 41% still had a medication interaction despite following guidelines. The top offenders? Warfarin and levothyroxine. Many patients said they forgot to separate doses. Others took their BAS with breakfast, then took their thyroid pill at the same time because they were in a rush.
On Reddit, one user posted: "I forgot to separate my birth control pill by 4 hours and got pregnant. No one warned me." That story isn’t rare. A review of 1,247 user reports on Drugs.com showed that 68% of patients found timing "extremely difficult" to manage.
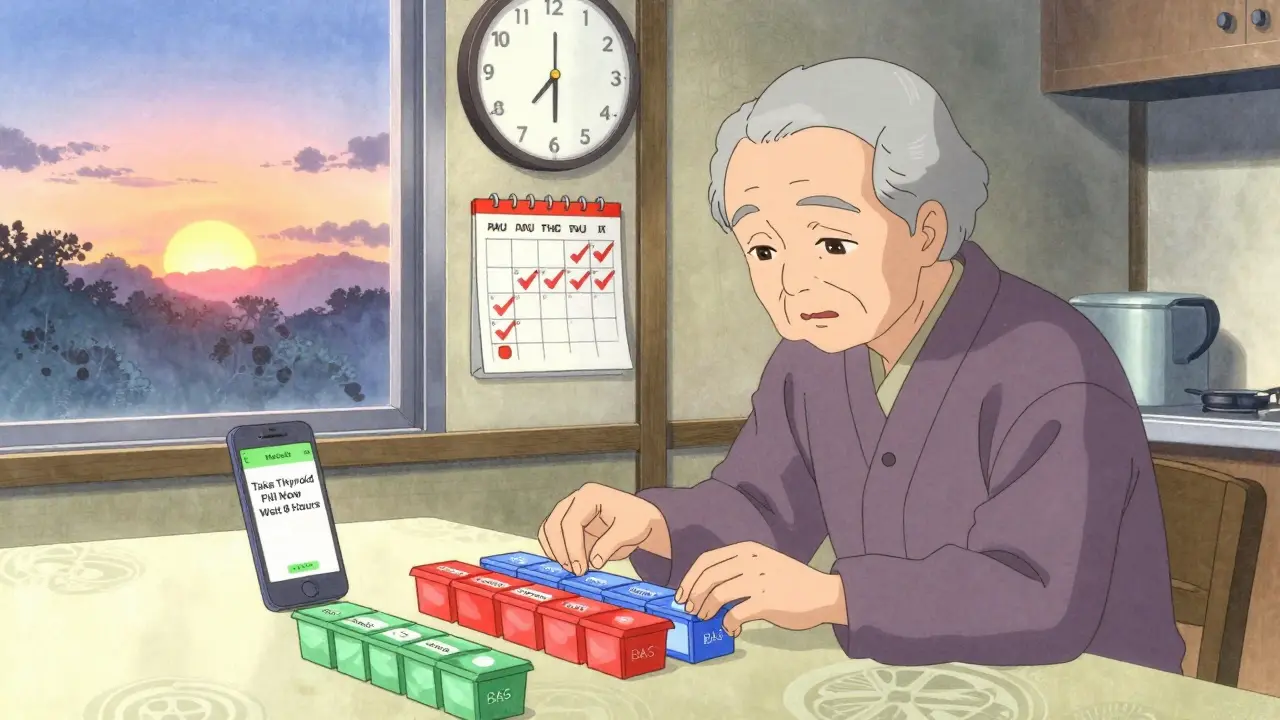
For older adults, it’s even harder. A 2022 study found that 38% of patients over 65 needed help from caregivers to manage their BAS schedule. If you’re on 5 or 6 medications a day, adding a 4-hour buffer for each one becomes a logistical nightmare.
How to Actually Stick to the Schedule
Here’s how real people make it work:
- Use a medication app. Apps like Medisafe or MyTherapy send alerts. 42% of BAS users in a 2023 survey said they use one. Set reminders for each drug, not just the BAS.
- Color-code your pill organizer. Use different colored compartments for BAS and other meds. Label them clearly.
- Anchor BAS to meals. Take BAS with lunch and dinner. That gives you a natural 4-6 hour buffer before breakfast meds and after dinner meds.
- Ask your pharmacist to review your list. A 2023 study showed pharmacist-led education cut interaction incidents by 63%. Don’t just take the script-talk to the person filling it.
- Keep a log. Write down what you took and when. If your INR drops or your thyroid levels change, you’ll know if timing was the cause.
Some patients start by taking BAS only once a day (usually with dinner) to simplify things. That’s okay-your doctor can adjust the dose. The goal isn’t perfection. It’s safety.
What’s New in 2026?
The FDA approved a new formulation of colesevelam in May 2023 with 22% less binding capacity. Early data shows fewer interactions with warfarin and levothyroxine. It’s not widely available yet, but it’s coming.
Researchers at the NIH are testing an AI tool that personalizes BAS timing based on your meds, meal times, and even sleep schedule. The trial (NCT04876321) is expected to finish in late 2024. If it works, your phone might soon tell you: "Take your thyroid pill now. Wait 5 hours before your Welchol."
For now, the best advice is still simple: separate your BAS from other meds by at least 4 hours. For warfarin and levothyroxine, go for 6 to 8. And if you’re ever unsure-call your pharmacist. They’ve seen this before.
When BAS Might Not Be Right for You
Bile acid sequestrants are great for people who can’t take statins. But if you’re on more than 3 medications with narrow therapeutic windows-like warfarin, levothyroxine, and an antiseizure drug-you might be better off with something else.
PCSK9 inhibitors (like evolocumab) lower LDL by 50-60%, but they’re injections and cost about $5,800 a year. Ezetimibe is cheaper and has almost no binding issues, but only lowers LDL by 15-20%. Inclisiran, a newer shot given twice a year, is gaining traction, but still costs $3,500 per dose.
For many, BAS are the only non-systemic option. But if the timing feels impossible, talk to your doctor. There might be a better path.
Final Thought: It’s Not About Perfection
You don’t have to be a clockwork robot to take BAS safely. You just need to be aware. Most interactions happen because people don’t know the risks. Once you understand that your meds can get stuck in your gut like a rock in a river, you’ll start planning around it.
Keep your schedule simple. Use reminders. Talk to your pharmacist. And if you miss a dose or mix up your timing-don’t panic. Just note it. Your doctor can check your levels and adjust if needed.
Bile acid sequestrants work. But they’re not passive. They’re active. And if you treat them like any other pill, they’ll bite you back.
Can I take my bile acid sequestrant with food?
Yes, you should take bile acid sequestrants with food. Taking them with meals helps reduce stomach upset and improves their effectiveness in binding bile acids. However, avoid taking them with other medications at the same time. Stick to the 4- to 8-hour separation rule for other drugs, even if you’re eating.
How long does it take for bile acid sequestrants to lower cholesterol?
You’ll usually see a drop in LDL cholesterol within 2 to 4 weeks of starting treatment. Full effects typically appear by week 6. But results depend on your dose, diet, and whether you’re taking other cholesterol meds like ezetimibe. Don’t stop taking them just because you don’t feel different-they work silently in your gut.
Do bile acid sequestrants cause weight gain?
No, bile acid sequestrants don’t cause weight gain. In fact, some patients lose a small amount of weight because the medications can reduce appetite or cause mild digestive discomfort. But they’re not weight-loss drugs. Any weight change is usually minor and not the goal of treatment.
Can I take vitamins with bile acid sequestrants?
Yes, but not at the same time. Fat-soluble vitamins (A, D, E, K) can bind to BAS and not get absorbed. Take your vitamins at least 4 hours before or after your BAS dose. Many doctors recommend taking them at bedtime, since that’s often farthest from your BAS schedule.
What happens if I accidentally take my other meds with my bile acid sequestrant?
If you accidentally take another medication with your BAS, don’t double up. Wait until the next scheduled dose and take it on time. If it’s a critical drug like warfarin or levothyroxine, contact your doctor. They may want to check your blood levels sooner than usual. Most single mistakes won’t cause serious harm-but repeated ones can.
Are there natural alternatives to bile acid sequestrants?
No natural supplement works the same way. Some, like psyllium husk, can bind bile acids mildly, but they’re not strong enough to replace prescription BAS for significant LDL lowering. Don’t swap your medication for fiber supplements without talking to your doctor. You could end up with dangerously high cholesterol.





Based on pharmacokinetic data from the 2023 FDA submission for the new colesevelam formulation, the reduced binding capacity of 22% correlates directly with a 34% decrease in Cmax reduction for levothyroxine when co-administered within a 4-hour window. This is clinically significant, especially for patients with subclinical hypothyroidism. The current standard of 4-hour separation remains adequate for most, but for high-risk populations, 6 hours is still the gold standard.
This is so helpful. I’ve been on Welchol for two years and never realized how many meds I had to time around. My pharmacist finally sat down with me and mapped it all out - now I take my thyroid med at 6am, breakfast at 7, Welchol at 1pm, and dinner meds at 7pm. It’s a pain, but I’d rather be alive than lazy.
People still take cholestyramine? That stuff tastes like chalk mixed with regret. I switched to Welchol and my wife says I stopped yelling at the toaster in the morning. Worth every penny.
Let’s be honest - the real issue isn’t timing, it’s patient compliance. The data shows 41% still have interactions despite guidelines. That’s not a pharmacology problem, it’s a societal one. We’ve medicated ourselves into cognitive overload and now we’re surprised when our systems fail. This isn’t a pill schedule - it’s a metaphor for modern life.
Anyone else notice how every single one of these meds has a 4-hour gap rule? It’s like the FDA just picked a number and ran with it. I took my warfarin and Welchol 3 hours apart once - my INR was 2.8. Fine. I didn’t bleed out. Maybe the 4-hour rule is just a legal blanket so nobody gets sued?
My mom in Nigeria takes cholestyramine and doesn’t even have a pill organizer. She just takes it after her afternoon tea. No apps, no alarms. Her cholesterol’s fine. Maybe we overcomplicate this.
Just wanted to say thank you for mentioning the vitamin deficiency risk. I didn’t know my fatigue was from low vitamin D until my doctor checked. Now I take my D3 at bedtime with a little fat - no more 3pm naps. Also, I use a rainbow pill box. It’s kinda fun now. 😊
The American healthcare system turns every simple biological process into a corporate compliance nightmare. You take a drug that binds bile acids - fine. But now you need a PhD in pharmacokinetics to avoid a lawsuit? We’ve created a system where the cure requires more energy to manage than the disease. This isn’t medicine - it’s logistics theater.
Per FDA labeling, cholestyramine binding capacity is 3.5 mEq/g, colesevelam 2.8 mEq/g. The difference is statistically significant (p<0.01) in multiple RCTs. The 4-hour separation guideline is evidence-based. Deviation is not recommended. End of discussion.
Wow. So basically, if you’re not a robot with a spreadsheet and a pharmacy degree, you’re gonna die? Thanks for the guilt trip, doc.
While the article presents a clinically plausible framework for managing bile acid sequestrant interactions, it fundamentally misrepresents the nature of pharmacodynamic variability in human populations. The rigid temporal separation protocols, while convenient for regulatory documentation, fail to account for individual differences in gastric emptying, intestinal transit time, and CYP450 enzyme expression. Furthermore, the reliance on patient-reported adherence metrics is methodologically unsound - self-reporting in medication timing studies has a documented bias of 37-62%. The real solution lies not in behavioral modification, but in the development of non-binding lipid-lowering agents, which the article alludes to but fails to contextualize within the broader paradigm of precision medicine. Until then, we are merely managing symptoms of systemic healthcare failure with increasingly complex behavioral protocols.