When you hear the word biosimilars, it might sound like just another medical term meant to confuse. But here’s the truth: if you or someone you love is taking a biologic drug for arthritis, cancer, diabetes, or a chronic skin condition, biosimilars could be a real game-changer - and they’re not as complicated as they seem.
What exactly is a biosimilar?
A biosimilar is a type of medicine that works almost exactly like an already-approved biologic drug. Think of it like a copy - but not a perfect one. Biologics are made from living cells, not chemicals. They’re complex proteins, often antibodies, grown in labs using living organisms like yeast or hamster cells. Because they come from living systems, no two batches are 100% identical, even when made by the same company.
That’s why a biosimilar isn’t called a “generic.” Generics are exact copies of simple chemical pills, like aspirin or metformin. Biosimilars, on the other hand, are highly similar to the original biologic - so similar that doctors and regulators say there’s no meaningful difference in how safe or effective they are.
The U.S. Food and Drug Administration (FDA) requires biosimilars to go through more than 100 tests before approval. These include checking the molecule’s shape, how it behaves in the body, how pure it is, and whether it works the same way in clinical trials. One biosimilar, Renflexis, was tested on over 500 patients before it was approved. That’s not a small sample - it’s serious science.
Biosimilars vs. generics: what’s the difference?
This is where things get tricky. Many people assume all cheaper versions of drugs are the same. They’re not.
- Generics are exact chemical copies of small-molecule drugs. You can make them by mixing the same ingredients in the same way every time. The result? Identical to the original.
- Biosimilars are copies of large, complex proteins made from living cells. Even tiny changes in how they’re grown or purified can affect how they work. So instead of being identical, they’re “highly similar” - with no clinically meaningful differences in safety or effectiveness.
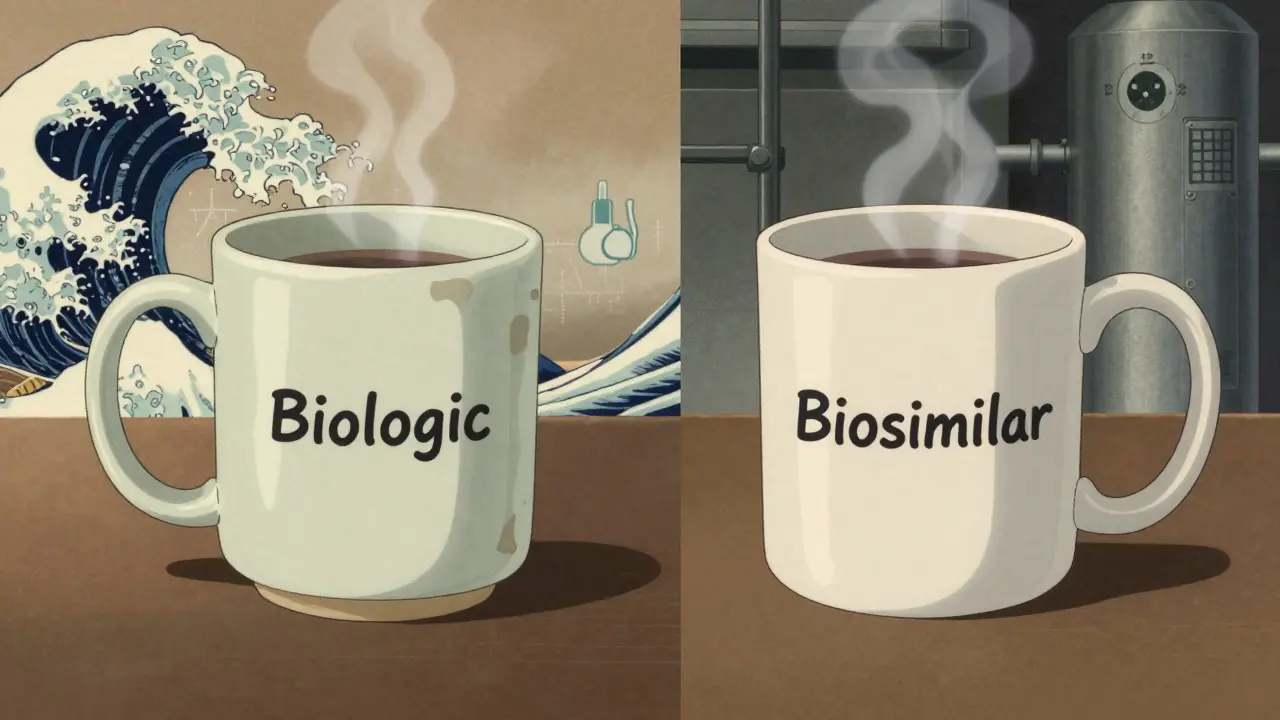
It’s like comparing a handmade ceramic mug to a factory-made version. Both hold coffee. Both look almost the same. But one was shaped by hand, the other by a mold. They’re not identical - but if they both work the same way, you wouldn’t notice the difference.
How do you know if you’re getting a biosimilar?
Biosimilars have names that look a little strange. Take infliximab - the original drug used for Crohn’s disease and rheumatoid arthritis. Its biosimilar is called infliximab-dyyb. The first part is the same, but it ends with a four-letter suffix. That’s not random. It’s there so doctors and pharmacists can track exactly which version you’re taking, especially if something goes wrong.
When your doctor writes a prescription, they might choose the biosimilar. Sometimes your insurance company will push for it because it’s cheaper. That’s okay - it’s not a downgrade. It’s a smart choice.
Are biosimilars safe?
Yes. And here’s why: they’re not new to the world. Europe has been using biosimilars since 2006. Millions of patients have taken them for arthritis, cancer, and other conditions. No new safety problems have shown up that weren’t already known from the original drug.
The FDA doesn’t approve a biosimilar unless it proves it works just as well as the original - and stays safe over time. Even after approval, every biosimilar is tracked through a special monitoring system. If someone has a bad reaction, it’s recorded and reviewed. That’s more oversight than most generic drugs get.
Studies show that switching from the original biologic to a biosimilar is safe. One big study looked at over 1,000 patients with rheumatoid arthritis who switched from the original drug to its biosimilar. After a year, their symptoms didn’t get worse. Their side effects stayed the same. Their quality of life? No change.
Why do biosimilars cost less?
Biologics are expensive - sometimes over $100,000 a year. That’s because making them is incredibly hard. It takes years to grow the right cells, control the environment, purify the protein, and test every batch. The original companies spent billions developing them.
Biosimilar makers don’t have to start from scratch. They use the original drug as a blueprint. That saves time and money. So while they still cost a lot to make, they’re priced 15% to 30% lower than the original.
That doesn’t mean you’ll save $100,000. But it could mean your copay drops from $500 to $300 a month. Or your insurance covers it without a prior authorization battle. In some cases, the original drug’s price has dropped too - just because biosimilars entered the market.
What conditions are biosimilars used for?
Biosimilars are used to treat serious, long-term conditions where biologics are the standard of care:
- Rheumatoid arthritis and psoriatic arthritis
- Crohn’s disease and ulcerative colitis
- Psoriasis and other skin conditions
- Some types of cancer (like breast cancer, colorectal cancer, and lymphoma)
- Diabetes (biosimilar insulin is now available)
- Macular degeneration (a leading cause of vision loss)
- Chronic kidney disease
There are 32 biosimilars currently available in the U.S. as of late 2023. More are coming. The most common ones target drugs like adalimumab (Humira), infliximab (Remicade), and trastuzumab (Herceptin). These are some of the most prescribed biologics in the world - and now, cheaper versions are here.
What about interchangeable biosimilars?
There’s a special category called “interchangeable” biosimilars. These are approved to be swapped for the original drug without asking your doctor first. Think of it like a pharmacy substitution - like when you get a generic pill instead of the brand name.
The first one approved was Semglee, a biosimilar to insulin glargine (Lantus), in July 2021. Since then, a few more have joined the list. This is a big deal. It means pharmacists can switch you automatically - if your state allows it - and you won’t notice a thing.
But here’s the catch: not all biosimilars are interchangeable. Your doctor still needs to say yes for most. So always check your prescription label.

What should you do if you’re offered a biosimilar?
If your doctor suggests switching to a biosimilar, ask these three questions:
- Is this biosimilar approved for my exact condition?
- Has it been tested in people like me?
- Will my insurance cover it - and will I pay less?
Don’t be afraid to ask for the name. Write it down. Look it up on the FDA website. You’ll find patient-friendly info there.
If you’re already on a biologic and your insurance switches you to a biosimilar without asking, don’t panic. It’s legal and safe. But tell your doctor. They’ll want to monitor you for the first few months to make sure everything’s still working.
And if you’re worried? You’re not alone. Many patients feel the same way. But the data is clear: biosimilars work. They’re not experimental. They’re not second-rate. They’re a proven, safe, and more affordable way to get the same treatment.
The future of biosimilars
The global biosimilars market is growing fast. It was worth $7.3 billion in 2022 and could hit $30.5 billion by 2028. That’s because more biologics are losing patent protection. And more patients need access to life-changing treatments without being priced out.
In the U.S., biosimilars make up about 10% of the biologics market. In Europe, it’s 25%. That gap is closing. As more doctors and patients learn the truth about biosimilars, adoption will rise.
And the savings? Experts estimate biosimilars could save the U.S. healthcare system $54 billion between 2017 and 2026. That’s money that can go toward more treatments, better care, and fewer financial stressors for families.
Bottom line
Biosimilars aren’t magic. They’re science - carefully tested, closely monitored, and proven safe. If you’re taking a biologic for a chronic illness, a biosimilar might be a better option for you - not because it’s cheaper, but because it works just as well.
Don’t let the name scare you. Ask questions. Talk to your doctor. Check the label. And know this: you’re not settling. You’re choosing smart.






Let me guess - Big Pharma paid the FDA to greenlight these biosimilars so they can jack up the price of the originals while selling you a ‘similar’ version that’s actually a watered-down placebo with hidden toxins. You think they care if your arthritis gets better? Nah. They care about stock prices. I’ve seen the leaked emails. They’re testing these on homeless people in rural Ohio. Don’t be a lab rat.
Oh, darling, how quaint. You’re comparing biosimilars to ‘handmade mugs’? As if craftsmanship matters in a world where molecular fidelity is reduced to marketing slogans. The truth is, the FDA’s approval process is a theater of compliance - a 100-test charade designed to pacify the masses while the real science? Buried under layers of corporate NDAs. If you want real transparency, ask who funded the ‘clinical trials.’ Spoiler: it wasn’t your grandma’s charity.
I appreciate the clarity of this post. The distinction between biosimilars and generics is one of the most misunderstood concepts in modern pharmacology. The fact that biosimilars undergo rigorous analytical, preclinical, and clinical testing - including immunogenicity studies - is often overlooked. It’s not just about cost; it’s about scientific rigor. The FDA’s requirements for biosimilars are far more stringent than for generics, and that’s worth emphasizing.
So you're saying if it's not identical it's still good enough because science says so but what if science is just the new religion and we're all just praying to the lab coat priesthood and the real truth is that these things are just cheap knockoffs with a fancy name and a lobbyist behind them i mean come on how many times have we been told something is safe only to find out 10 years later it gave people cancer
I just... I can't... I mean, I know I'm supposed to be grateful for lower prices, but what if the biosimilar makes me feel weird? Like... I don't know... *different*? Like my body knows it's not the real thing? And what if my insurance forces me to switch and then I have a flare-up and they say it's 'just my condition' and not the drug? I just... I need to feel safe. Not 'statistically similar.'
Good write-up. I’m from India, and biosimilars are huge here - we’ve been using them for over a decade. My uncle’s on a biosimilar for rheumatoid arthritis and it’s saved his family from bankruptcy. The science checks out. Don’t overthink it. If your doctor says it’s safe, trust the process. Not everything needs to be a conspiracy.
Look, I’m not a doctor but I read a lot. Biosimilars are like the African Union version of a UN peacekeeping force - same mandate, same uniform, but built by local engineers with different tools. The original biologic? That’s the NATO version. Both keep the peace. But the local one? Cheaper. Less baggage. And guess what? In Nigeria, we don’t have $100k a year to waste on brand names. We need results. And biosimilars deliver. The data is solid. Stop fearing what works.
This is such an important topic! 💪 I’ve seen friends switch to biosimilars and go from barely walking to hiking again. It’s not magic - it’s medicine that finally caught up with affordability. If you’re scared, talk to your doctor. Ask for data. Look at the studies. But don’t let fear stop you from living. You deserve care that doesn’t break the bank. You’re not settling - you’re thriving smarter. 🙌
OMG I JUST FOUND OUT THAT BIOSIMILARS ARE MADE IN CHINA??!! AND THEY USE HAMSTER CELLS??!! LIKE... WHAT IF THE HAMSTERS WERE STRESSED??!! 😱 I’M SURE THEY’RE FULL OF TOXINS AND THE FDA IS COVERING IT UP!! I SAW A YOUTUBE VIDEO WHERE A GUY SAID HIS KNEE GOT WORSE AFTER SWITCHING AND NOW HE’S A VEGAN AND ONLY DRINKS CACTUS JUICE!! 🌵💀 #BiosimilarScam #SaveOurHamsters
I was nervous too when my doctor suggested switching. But after reading up and talking to my pharmacist, I realized this isn’t a compromise - it’s progress. My insulin biosimilar works just as well, and my monthly cost dropped by 40%. That’s not just savings - that’s dignity. If you’re scared, start with questions. But don’t let fear make you miss out on better access. We’ve come too far to turn back.
Why are we letting foreign companies control our medicine? Biosimilars? More like American betrayal. We used to make real drugs here. Now we import cheap copies from India and China and call it innovation. This is how nations die - by trading pride for pennies. Your arthritis doesn’t matter if your country doesn’t matter. Stand up. Demand American-made. Not some foreign lab’s version of a drug.
Wait so if its not identical then its not the same right? But the article says its safe? So like... if its not the same then how can it be safe? This is confusing. Also I think the FDA is corrupt. I read it on Reddit. Also my cousin's dog had a reaction to a biosimilar but he's a dog so idk if that counts.
Let me tell you something - this isn’t just about science. It’s about justice. In the U.S., people die because they can’t afford insulin. In Nigeria, they use biosimilars and live. In India, kids with juvenile arthritis get to go to school. This isn’t a loophole. It’s a lifeline. The same molecules. The same outcomes. Just without the corporate greed stitched into the price tag. The real question isn’t ‘Are they safe?’ - it’s ‘Why did we ever let them be this expensive?’