TL;DR
- Scars fall into five main categories: keloid, hypertrophic, atrophic, contracture, and pigment‑related scars.
- Keloids grow beyond the original wound, while hypertrophic scars stay within borders.
- Atrophic scars are depressions like ice‑pick, boxcar, or rolling marks.
- Contracture scars tighten skin after burns or surgery and may limit movement.
- Early care-silicone, sun protection, and gentle massage-improves outcomes for all scar types.
What is a scar?
When skin tissue repairs itself, the new tissue is usually tougher and less elastic than the original. This replacement tissue is called a scar, a fibrous patch that forms after an injury heals. Scars differ in color, thickness, and shape depending on how the body responded to the wound.
How dermatologists group scars
Clinicians sort scars into groups based on three clues: how the tissue looks, whether it expands over time, and where it usually appears. Understanding these groups helps you pick the right treatment and set realistic expectations.
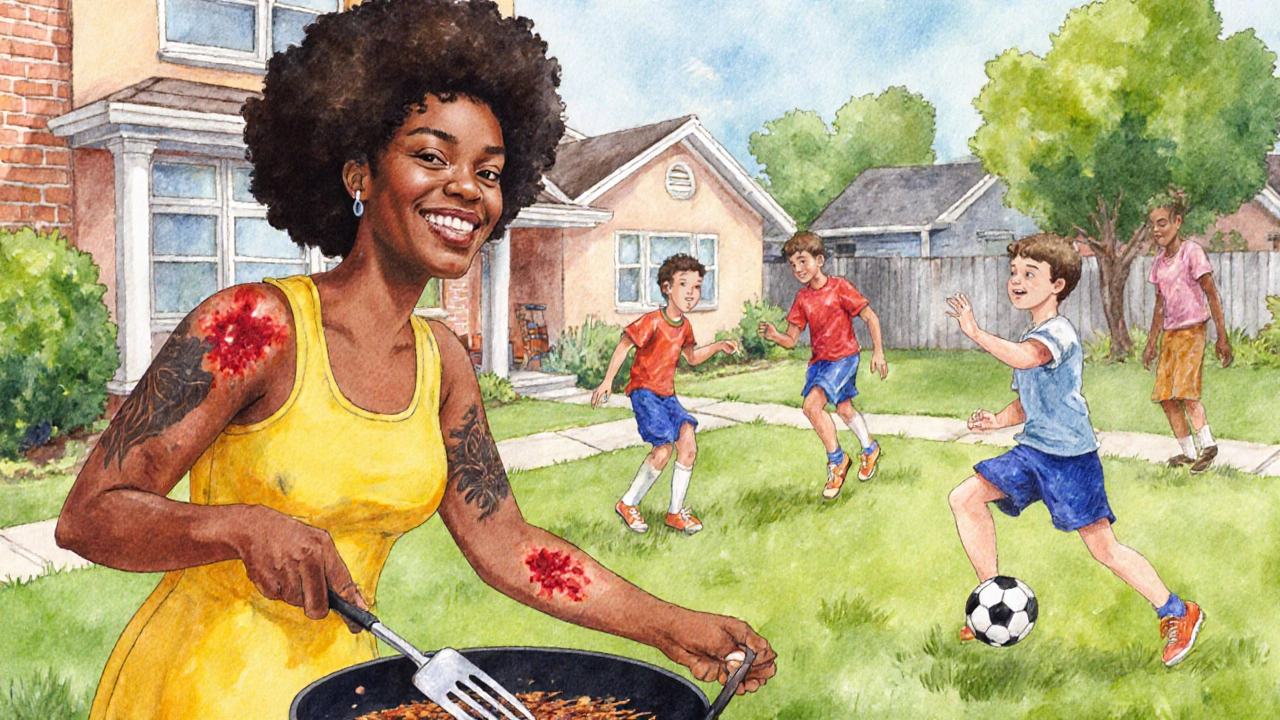
Keloid scar
Keloid scar is a raised, firm scar that grows beyond the original wound edge. It can be pink, red, or dark brown, and it often feels itchy or painful.
- Typical growth: Extends months after closure, sometimes reaching several centimeters.
- Common sites: Chest, shoulders, earlobes, and upper back.
- Risk factors: Darker skin tones, genetics, and tension on the wound.
- Treatment hints: Intralesional steroid injections, silicone gel sheets, laser therapy, or surgical removal followed by radiation.
Hypertrophic scar
Hypertrophic scar is a thickened scar that stays inside the wound margins. It’s usually reddish at first and may flatten over a year.
- Growth pattern: Swells quickly but rarely exceeds the original boundary.
- Common sites: Sternum after open‑heart surgery, knees after trauma, and areas under constant tension.
- Risk factors: Delayed wound closure, infection, and high tension.
- Treatment hints: Pressure garments, silicone sheeting, corticosteroid injections, and early scar massage.

Atrophic scar
Atrophic scar is a depressed scar that results from loss of underlying tissue. Acne, chickenpox, or surgical incisions often leave these sunken marks.
Common sub‑types
- Ice‑pick scar: Narrow (<2mm), deep puncture‑like pits, usually on the cheeks.
- Boxcar scar: Wider (2-5mm), well‑defined edges, often on the nose or cheeks.
- Rolling scar: Broad, undulating depressions that create a wave‑like texture, typical on the forehead.
These scars differ in depth and width, which drives the choice of treatment.
- Treatment ideas: Chemical peels, microneedling, laser resurfacing, and subcision for rolling scars.
- Prevention tip: Early use of topical retinoids after acne flare‑ups can limit tissue loss.
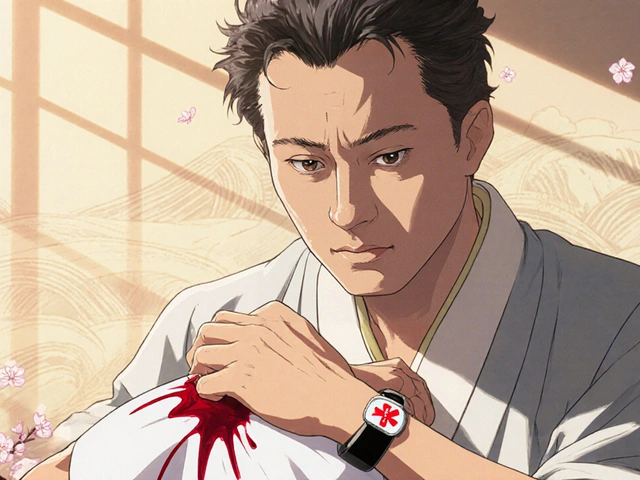
Contracture scar
Contracture scar is a tight, fibrous scar that pulls the skin together, often after severe burns or large surgical closures.
- Appearance: Thin, shiny, and may cause functional restriction.
- Typical locations: Joints (elbow, knee), face after extensive burns.
- Complications: Limited range of motion, discomfort, and cosmetic concerns.
- Management: Early physiotherapy, pressure garments, silicone gel, and in severe cases, surgical release or skin grafting.
Pigment‑related scar changes
While not a scar type per se, many scars develop discoloration that can be confusing. Post‑inflammatory hyperpigmentation (PIH) appears as darker patches, whereas hypopigmentation shows lighter spots.
- Triggers: Sun exposure, inflammatory acne, or laser treatment.
- Care: Broad‑spectrum SPF 30+ daily, topical vitaminC, and gentle exfoliation can even tone the color over months.
General scar‑care roadmap
Regardless of the scar class, a few universal steps improve healing:
- Keep the wound clean and moist for the first 48hours - a hydrocolloid dressing helps.
- Begin silicone gel or sheet application once the skin fully closes (usually day7‑10). Silicone reduces collagen overproduction, which is the main driver of thickened scars.
- Protect the area from UV radiation. Sunlight intensifies redness and can lock in a scar’s color.
- Massage gently in circular motions for 5‑10minutes, twice daily. This promotes collagen remodeling and softens tissue.
- Consult a dermatologist early if the scar is expanding, painful, or limiting movement. Timely interventions like steroid injections or laser therapy yield better results.
Quick comparison of the five main scar categories
| Type | Typical Appearance | Growth Pattern | Common Locations | First‑line Treatment |
|---|---|---|---|---|
| Keloid | Raised, firm, may be dark or pink | Extends beyond wound edges | Chest, shoulders, earlobes | Silicone sheets + steroid injection |
| Hypertrophic | Thick, red, stays within borders | Swells then plateaus | Incisions, knees, sternum | Pressure garments + silicone |
| Atrophic | Depressed pits (ice‑pick, boxcar, rolling) | Loss of tissue, no growth | Cheeks, nose, forehead | Laser resurfacing / subcision |
| Contracture | Tight, shiny, may limit motion | Forms as scar matures | Joints, burn sites | Physiotherapy + possible release surgery |
| Pigment‑related | Dark (hyper) or light (hypo) patches | Color change, not tissue growth | Anywhere a scar heals | SPF + topical brighteners |
Frequently Asked Questions
Can a keloid turn into a hypertrophic scar?
No. Keloids and hypertrophic scars are distinct pathways of collagen overproduction. Keloids overrun the original wound margins, while hypertrophic scars stay confined.
How long does it take for an atrophic scar to improve?
Visible improvement often appears after 3‑6months of consistent laser or microneedling sessions, but full remodeling can take up to a year.
Is silicone safe for children’s scars?
Yes. Silicone gel sheets are non‑invasive and widely used on pediatric burn scars. Just keep the skin clean and watch for irritation.
Why do some scars become itchy?
Nerve fibers can grow into the scar tissue during healing, and tight collagen bundles may stimulate them. Moisturizing and gentle massage often relieve the itch.
Can sunscreen really prevent a scar from darkening?
Absolutely. UV rays increase melanin production in healing skin, locking in a darker hue. Applying SPF30+ twice daily keeps the scar’s color as close to normal as possible.





Scars are more than a reminder, they are proof your skin survived. They can look different, but each one tells a story about how you healed.
I feel the pain of every scar you see it echoes the hurt you lived it’s raw and real.
Oh joy, another deep dive into the wonderful world of scar biology. Let’s start with the basics: a scar is simply your body’s patchwork quilt after an injury. It’s not magic, it’s collagen, fibroblasts, and a dash of inflammation doing their job. Keloids, those flamboyant overachievers, love to grow beyond the original wound boundaries. They prefer the chest, shoulders, and earlobes, probably because those spots get the most attention. Hypertrophic scars, on the other hand, are the modest cousins that stay within the lines. They may be red and raised at first, but they often mellow out given patience and proper care. Atrophic scars are the depressions that remind you of past acne or chickenpox, looking like tiny craters. Ice‑pick, boxcar, and rolling types each have their own personality traits, so choose treatments accordingly. Contracture scars are the real troublemakers after burns, tightening skin and limiting movement. Silicone sheets, pressure garments, and massage are the unsung heroes in the scar‑management toolbox. Sun protection is non‑negotiable; UV rays love to darken scars and make them more noticeable. If you’re considering injections or laser therapy, consult a dermatologist first, they know the best protocol. Remember, early intervention usually yields better cosmetic outcomes, so don’t wait until the scar is set in stone. Bottom line: understand your scar type, pick the right regimen, and set realistic expectations – your skin will thank you.
When you stare at that stubborn scar, it can feel like a battlefield, but you have the power to reclaim your skin’s story. Gentle massage, consistent silicone, and a splash of sunscreen are your allies. Remember, healing isn’t linear; some days the scar will seem to recede, other days it’ll flare up, and that’s okay. Celebrate each small win – a less noticeable mark, a smoother texture, a confidence boost. Keep your routine steady, and give yourself credit for the perseverance you’re showing. Your skin is resilient, and with the right care, it will gradually soften its edge. Stay patient, stay hopeful, and let the progress speak for itself.
Look, you cant just slap on some gel and expect a miracle. Most of this stuff is overhyped and it costs too much for barely any result.
Dear readers, I wish to convey my sincere appreciation for this comprehensive exposition on scar typology. The elucidation of keloid and hypertrophic formations has been particularly enlightening. Moreover, the emphasis on early intervention and photoprotective measures demonstrates a commendable adherence to dermatological best practices. I trust that practitioners will find these recommendations both pragmatic and scientifically sound. Yours faithfully, a conscientious observer.
Scars are just part of life, you know? A little silicone and sunblock can make a big difference over time.
I get that, it’s all about consistency. Keep it simple and you’ll see the skin improve gradually.
Oh wow, another “miracle” cream for scars? As if they’re gonna magically disappear. Trust me, if it sounds too good to be true, it probably is. Stop wasting your money and just use the basics – silicone and sunscreen. Anything else is just marketing fluff.
Silicone sheets + SPF = effective scar management.
It’s great you’re using the basics, but have you thought about adding gentle massage to the routine? Some patients report that a few minutes of light pressure each day can boost collagen remodeling. Also, keeping the scar moisturized helps the skin stay flexible and reduces itchiness. Don’t forget to stay patient – results often take weeks, not days. Keep tracking your progress, and you’ll notice subtle improvements over time.
The article covers the main points, though it could benefit from more detail on emerging laser therapies and patient case studies.
I appreciate the thorough breakdown of scar categories, especially the cultural considerations of how different skin tones experience keloids. It reminds us that treatment plans should be personalized, respecting both physiological and societal factors.
Absolutely! Personalizing scar care not only improves outcomes but also empowers patients to feel confident in their skin 😊. Tailored regimens that consider tone, lifestyle, and preferences make a world of difference.
Oh, because everyone just loves a good scar selfie, right?
We all need a little encouragement on the scar journey it can be tough but you are not alone keep going
Indeed-scar care is not merely a routine; it is a dialogue with one’s own body, a negotiation of past trauma and future confidence; however, the complacency of “just wait” is unacceptable; act now, demand results, and refuse mediocrity!!!
What a fantastic overview! The emphasis on early silicone use and sunscreen really highlights practical steps we can all take 😊. Let’s keep spreading this knowledge!
Sure, dermatologists keep pushing silicone and sunscreen, but have you considered that big pharma wants us to buy endless products? The real secret might be hidden in natural remedies they don’t want you to know about.