Spina Bifida Risk Assessment Tool
This tool helps evaluate potential risk factors for spina bifida. Please answer the following questions honestly to get a personalized risk assessment.
Your Risk Assessment
When a doctor spots an abnormality on a mid‑pregnancy scan, parents often wonder what it means for the child’s future. Spina bifida is a neural tube defect that occurs when the backbone and spinal cord don’t close completely during early embryonic development. The condition can range from a thin flap of skin covering the opening to a severe form called myelomeningocele where the spinal nerves protrude through the defect, often causing paralysis and organ problems. Because the spinal cord is involved, many parents worry about the child’s brain and learning abilities. Below we break down what the science says, how early detection changes the story, and what families can do to give their child the best start.
Key Takeaways
- Spina bifida is diagnosed in about 1 in 1,000 births in the U.S., and prenatal imaging catches roughly 80% of cases.
- The most common cognitive impact is reduced processing speed, not a global IQ drop.
- Early surgery-either in‑utero or within the first few months-lowers the risk of hydrocephalus and improves motor outcomes, which indirectly supports learning.
- Folic acid supplementation before conception can prevent up to 70% of spina bifida cases.
- Ongoing developmental monitoring and tailored early‑intervention programs are crucial for maximizing cognitive potential.
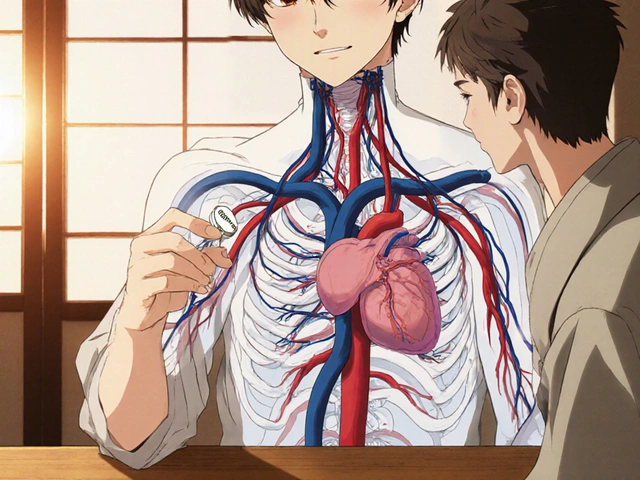
Understanding the Defect: From Embryo to Birth
The neural tube forms between days 22 and 28 after conception. If it fails to close, a gap remains in the vertebral column. This gap is what we call neural tube defect a birth anomaly that includes spina bifida, anencephaly, and encephalocele. The severity depends on where along the spine the opening occurs and whether the spinal cord tissue is exposed.
In most cases, the defect is located in the lower back (lumbar or sacral region). When the opening is small, a thin membrane covers the nerves, leading to milder motor issues. With myelomeningocele, the nerves are exposed, raising the chance of nerve damage and secondary complications like bladder dysfunction and orthopedic problems.
How We Spot Spina Bifida Before Birth
Modern obstetrics offers two main imaging tools:
- Prenatal ultrasound a sound‑based scan performed around 18‑20 weeks that can visualize the spine, detect the classic "lemon sign" in the skull, and show the "banana sign" of the cerebellum.
- Fetal MRI a magnetic‑resonance scan used after 20 weeks to provide detailed images of brain structures and spinal cord involvement.
Ultrasound is the frontline tool because it’s widely available and cheap. When the scan suggests spina bifida, a fetal MRI can confirm the diagnosis, map the exact level of the defect, and assess associated brain changes such as ventriculomegaly (enlarged fluid spaces) that signal hydrocephalus risk.
Why the Brain Matters: Cognitive Development Explained
Spina bifida doesn’t directly damage the brain, but the condition can set off a cascade that affects learning:
- Hydrocephalus: About 70% of children with myelomeningocele develop excess cerebrospinal fluid, which puts pressure on the cerebral cortex. If untreated, this pressure can slow down neural processing.
- Mobility limitations: Limited ability to explore the environment reduces opportunities for learning through play, which in turn can affect language and problem‑solving skills.
- Medical interventions: Frequent surgeries and hospital stays can disrupt routine, making it harder to establish consistent educational routines at home.
Research from a 2023 longitudinal study of 312 children with spina bifida showed that the average IQ was roughly 5‑7 points lower than sibling controls, but the gap narrowed when hydrocephalus was surgically managed early. More strikingly, processing speed (how quickly a child can take in and use information) was reduced by about 15% on average, while verbal comprehension remained on par with peers.

Early Intervention: Surgery and Its Ripple Effects
There are two timing options for repairing the defect:
- In‑utero repair: Performed between 19‑26 weeks via fetoscopic or open surgery, this approach reduces the need for post‑natal shunting by ~40% and improves lower‑limb motor function.
- Post‑natal repair: Done within the first few days after birth, it still offers protection against infection but doesn’t lower shunt rates as effectively.
When a ventriculoperitoneal shunt is placed to treat hydrocephalus, studies show that children who receive the shunt before six months of age tend to have better academic outcomes than those who wait longer. The reason is simple: maintaining normal intracranial pressure supports the growth of white‑matter pathways critical for reading and math.
Preventing Spina Bifida: The Power of Folate
One of the most actionable pieces of advice comes from a public‑health triumph: daily folic acid a B‑vitamin (400µg) that helps close the neural tube during early pregnancy. Women who start supplementation at least one month before conception cut their risk of having a baby with spina bifida by up to 70%.
For families with a previous child affected by a neural tube defect, a higher dose (4mg) is often recommended. Genetic counseling can also identify rare mutations in the MTHFR gene that affect folate metabolism, allowing doctors to tailor the supplementation plan.
Monitoring Development: What Parents Should Watch For
Once the baby is born, the first two years are critical. Here’s a practical checklist:
| Age | Milestone | Potential Red Flag |
|---|---|---|
| 6months | Sits without support | Persistent trunk instability |
| 12months | First words, crawls | Limited vocalizations or delayed crawling |
| 24months | Combines two words, walks confidently | Frequent falls or speech that lags two‑step behind peers |
| 3‑5years | Preschool readiness (color naming, basic counting) | Difficulty following multi‑step instructions |
Regular neuropsychological testing-ideally once a year until school age-helps catch subtle processing‑speed issues early. Early‑intervention programs that focus on motor skills, language enrichment, and visual‑spatial games have shown measurable gains in IQ‑equivalent scores.
Practical Tips for Parents and Caregivers
- Build a multidisciplinary team: Pediatric neurosurgeon, developmental pediatrician, physical therapist, and speech‑language pathologist should all be in the loop.
- Use assistive tech: Tablet apps that reinforce visual‑spatial reasoning can offset processing‑speed delays.
- Stay consistent with therapy: Short, daily motor exercises are more effective than a once‑weekly hour‑long session.
- Advocate at school: Request an Individualized Education Program (IEP) that includes extra time on tests and access to a classroom aide.
- Watch hydration and bladder health: Urinary infections can exacerbate cognitive fatigue, so proactive catheter care is a must.
Long‑Term Outlook
With modern prenatal care, early surgery, and robust developmental support, many children with spina bifida attend college, work full‑time, and lead independent lives. The median life expectancy in the U.S. now exceeds 60years, up from 30years a few decades ago.
What changes the equation most? Early detection, proactive shunt management, and a family that treats the child’s learning needs as a priority, not an afterthought.

Frequently Asked Questions
Can spina bifida be cured?
There’s no cure that erases the defect, but surgery can close the opening, prevent infection, and reduce the need for shunts. Combined with early‑intervention services, most children achieve functional independence.
Is prenatal ultrasound always accurate?
Ultrasound catches about 80% of cases, but some subtle forms require fetal MRI for confirmation. A missed diagnosis is rare when standard 18‑20‑week scans are performed.
How much folic acid should a woman take?
The general recommendation is 400µg daily, starting at least one month before conception. For a previous birth with a neural tube defect, a doctor may prescribe 4mg per day.
Will my child need special education?
Not necessarily, but many families benefit from an IEP that provides accommodations like extra test time, assistive technology, and physical‑therapy breaks during the school day.
What are the biggest risks after surgery?
Infection, shunt malfunction, and tethered‑cord syndrome are the primary concerns. Regular follow‑up imaging and prompt attention to headaches or changes in bladder function help catch problems early.




Reading this really hits home 😢. It’s tough seeing how spina bifida can shape a child’s learning journey, but early support makes a huge difference. I’ve known families who turned the odds around with therapy and love. Remember that a caring environment can boost confidence. Keep the conversation open and compassionate. 🙏
From a neurodevelopmental standpoint, the interruption of the neural tube can lead to altered cortical connectivity, which may manifest as deficits in executive function, language processing, and sensorimotor integration. Prenatal folic acid supplementation reduces the incidence of these malformations by up to 70%, highlighting the importance of periconceptional interventions. Moreover, intra‑uterine surgery has shown promise in mitigating hindbrain herniation, thereby improving long‑term cognitive outcomes. Early multidisciplinary assessment, including neuroimaging and standardized developmental testing, is essential for individualized care planning.
It’s heartbreaking but also hopeful. Simple things like a calm routine and gentle encouragement can help kids with spina bifida develop stronger reading and problem‑solving skills. Small wins add up, so celebrate every milestone.
Totally agree with the need for early intervention. A friendly vibe at home and consistent speech therapy can make a world of difference for these little ones.
Life throws curveballs, but philosophy teaches us to find meaning in the struggle. When a baby faces spina bifida, it’s a reminder to cherish every moment and nurture curiosity, no matter the obstacles.
Spina bifida can affect brain development in many ways. The condition may limit the flow of neural signals. That can lead to slower processing speed. Some children struggle with memory tasks. Language skills might develop later than peers. Motor coordination can also be impacted. Early assessment helps identify specific needs. Physical therapy can improve strength and balance. Speech therapy supports language growth. Occupational therapy aids daily living skills. A supportive family environment boosts confidence. Regular school accommodations provide necessary help. Monitoring progress guides therapy adjustments. Collaboration between doctors and educators is vital. Positive outlook and consistent care make a big difference.
Wow, such a vivid picture! Your words paint a rainbow over a stormy sea. It’s amazing how compassion can turn challenges into colorful opportunities. Keep shining that bright light.
The presented assessment tool appears thorough, yet its user interface lacks clarity. It would benefit from a concise instructional preamble and more accessible language for laypersons. Additionally, incorporating a feedback mechanism could enhance user confidence in the results.
While the tool seems practical, one might argue that the underlying assumptions ignore socioeconomic disparities. Nevertheless, it remains a decent starting point for informed discussions.
From a clinical perspective, the risk matrix aligns with current epidemiological models. However, we must emphasize that folic acid adherence remains the cornerstone of prevention. Advanced imaging protocols can further stratify risk, guiding both obstetricians and neurologists in prenatal counseling.
Great summary! Staying optimistic and keeping an eye on the latest research can really empower families dealing with spina bifida.