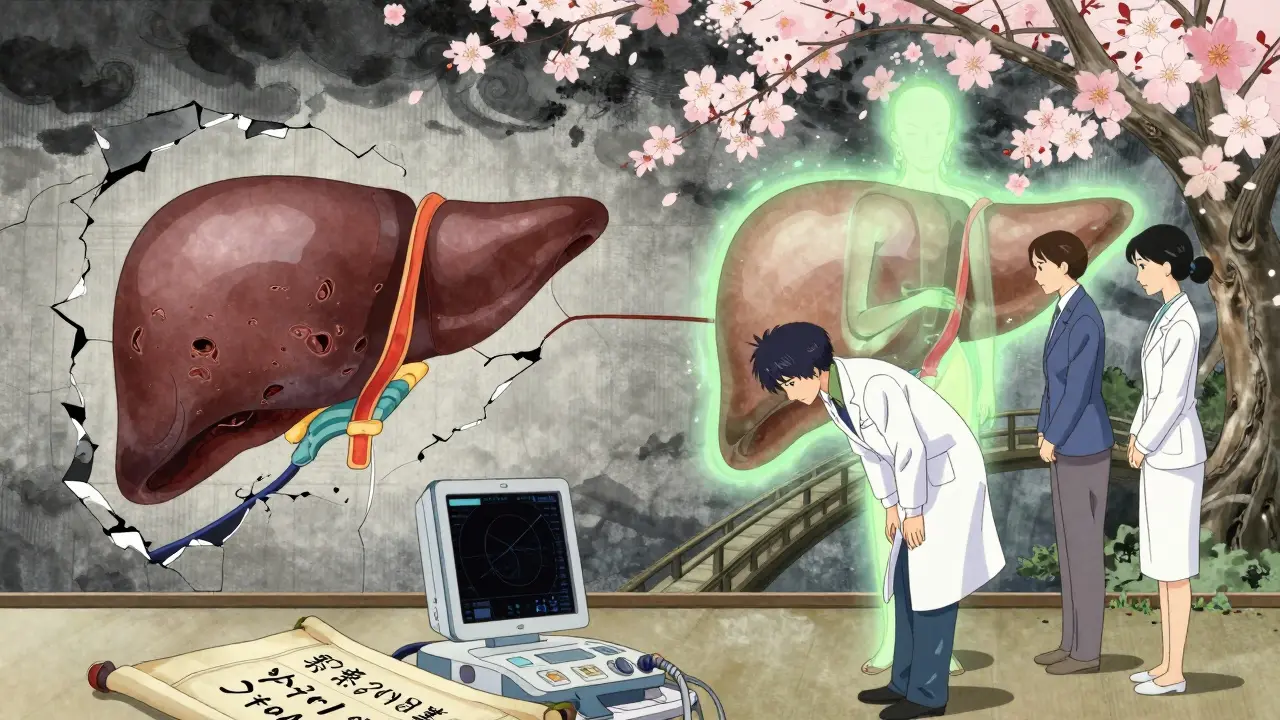
When your liver starts storing too much fat, it’s not just about being overweight - it’s a metabolic signal your body is out of balance. Metabolic-Associated Fatty Liver Disease, now called MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease), affects nearly one in three adults worldwide. It’s not caused by alcohol. It’s caused by insulin resistance, belly fat, high blood sugar, and high triglycerides. And here’s the hard truth: if you don’t do something about it, 20% of people with MASLD will develop liver inflammation, scarring, and even cirrhosis within a decade.
What MASLD Really Means
The name change from NAFLD to MASLD in 2023 wasn’t just semantic. It shifted the focus from excluding other causes to actively diagnosing metabolic dysfunction. If you have more than 5% fat in your liver and at least one metabolic issue - like obesity, type 2 diabetes, high blood pressure, or abnormal cholesterol - you have MASLD. No more guessing. No more exclusionary tests. It’s a diagnosis based on what’s happening inside your body, not what’s not happening.
Think of your liver as a storage warehouse. Normally, it handles fats efficiently. But when your fat cells become insulin resistant, they dump too many free fatty acids into your bloodstream. Your liver, overwhelmed, turns those fats into triglycerides and stores them. On top of that, your liver starts making its own fat from sugar - especially fructose - at a rate that’s 26% higher than normal. Add in poor fat burning and slow export, and you’ve got a perfect storm.
Weight Loss Isn’t Optional - It’s the Foundation
There’s no magic pill that replaces weight loss for MASLD. But the good news? You don’t need to lose 50 pounds. The science is clear: losing just 5% of your body weight reduces liver fat. Losing 7% improves inflammation. And if you hit 10%? That’s when liver scarring can actually reverse.
The Look AHEAD trial showed people who lost 10% of their weight cut their risk of developing the more dangerous form, MASH, by 90%. That’s not a small win. That’s life-changing. How? When you lose weight, your fat cells stop leaking fatty acids. That cuts the main source of liver fat by 30-40%. Your liver also stops making as much fat from sugar, and it gets better at burning fat for energy.
The European guidelines recommend losing 7-10% of your body weight over 6-12 months. That’s about 1-2 pounds per week. Combine it with 150-300 minutes of walking, cycling, or swimming each week, and you’re doing more than just shrinking your waistline - you’re healing your liver.

GLP-1 Drugs: The Game-Changer
For many people, losing 10% of their weight through diet and exercise alone is incredibly hard. That’s where GLP-1 receptor agonists come in. These drugs - like semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda) - were originally designed for diabetes. But their weight loss effect turned them into a breakthrough for MASLD.
Semaglutide, at 2.4 mg per week, helped people lose an average of 15% of their body weight in clinical trials. In one study, 55% of MASLD patients saw a major drop in liver fat after 68 weeks. Liraglutide helped 39% of patients reverse MASH - nearly double the placebo rate.
These drugs don’t just make you feel full. They work on multiple levels: they improve insulin sensitivity in fat tissue, reduce fat production in the liver by 20-25%, and calm down liver inflammation by blocking NF-κB, a key inflammatory switch. In the REGENERATE trial, semaglutide at 1.0 mg per week led to MASH resolution in 52% of patients - compared to just 22% on placebo.
Real People, Real Results - and Real Challenges
Not everyone’s experience is smooth. On patient forums, 76% of people using semaglutide reported nausea. About 32% quit within six months because the side effects were too much. Others found their appetite came back after stopping, and they regained most of the weight.
But there are success stories too. One person on HealthUnlocked lost 12.3% of their weight over nine months with semaglutide. Their FibroScan showed liver fat dropped from 328 to 245 dB/m - a clear sign of improvement. The key? They didn’t just take the shot. They worked with a dietitian, followed a Mediterranean-style diet with less than 25g of fructose per day, and stayed active.
Adherence jumps from 42% to 65% when medication is paired with structured dietary support. That’s the real lesson: GLP-1 drugs aren’t a shortcut. They’re a tool - and they work best when used with real lifestyle changes.
What’s Next? The Future of MASLD Treatment
The market for MASLD treatments is exploding. It’s expected to hit $28 billion by 2030. Semaglutide leads the pack, but tirzepatide (Mounjaro) is coming close - with even better weight loss numbers in early trials.
The FDA just approved resmetirom for MASH, expected in early 2024. This drug targets liver-specific pathways and may help patients with advanced scarring - where GLP-1 drugs have less impact. Some experts are already talking about combining resmetirom with semaglutide: one drug to reduce fat and inflammation, the other to heal fibrosis.
But access is still uneven. While 72% of U.S. academic hospitals now have MASLD clinics, only 28% of rural counties have any specialist at all. And cost remains a barrier. Semaglutide runs about $1,350 a month. Medicare covers it for obesity in 67% of cases - but many private insurers still fight it.
What You Can Do Right Now
If you’ve been diagnosed with MASLD, here’s what to do:
- Get a FibroScan or MRI-PDFF to measure liver fat and stiffness. Don’t rely on ALT levels - they’re often normal even when damage is happening.
- Set a realistic weight goal: aim for 7-10% loss over the next year. Break it into 1-2 pound weekly targets.
- Work with a dietitian. Focus on whole foods, fiber, healthy fats, and cut added sugar - especially fructose from soda and processed snacks.
- Move daily. 30 minutes of brisk walking five times a week is enough to start.
- If lifestyle changes aren’t enough after 6 months, talk to your doctor about GLP-1 agonists. Don’t wait until your liver is severely scarred.
There’s no cure for MASLD - but there is a path to reversal. And it starts with two things: losing weight and staying consistent. GLP-1 drugs can help you get there faster. But they’re not a replacement for the foundation. They’re the rocket booster - not the engine.
Can you reverse MASLD without medication?
Yes - but only if you lose at least 10% of your body weight. Studies show that 45% of people who achieve this level of weight loss see MASH resolve. It’s harder without medication, but it’s possible with sustained diet, exercise, and behavior change. Many people do it - but most struggle to keep the weight off long-term.
Do GLP-1 drugs work for everyone with MASLD?
Not always. They work best for people with obesity, type 2 diabetes, or prediabetes. They’re less effective if you already have advanced fibrosis (F3-F4). In those cases, newer drugs like resmetirom may be needed. Also, about one-third of people can’t tolerate the side effects - nausea, vomiting, or diarrhea - and stop taking them.
How long do you need to take GLP-1 drugs for MASLD?
There’s no fixed timeline. MASLD is a chronic condition tied to metabolism. If you stop the drug, you’ll likely regain weight - and liver fat will return. Most experts recommend staying on it as long as you benefit and can tolerate it. Think of it like blood pressure medication: you take it because you need it, not because you’re cured.
Is MASLD the same as alcoholic fatty liver?
No. MASLD is caused by metabolic problems - insulin resistance, belly fat, high blood sugar. Alcoholic fatty liver is caused by drinking too much alcohol. The liver damage looks similar, but the causes are completely different. That’s why the old term NAFLD (non-alcoholic fatty liver) was misleading. MASLD makes it clear: it’s about your metabolism, not your drinking habits.
Can you use GLP-1 drugs if you don’t have diabetes?
Yes. Semaglutide (Wegovy) and liraglutide (Saxenda) are FDA-approved specifically for weight management in people without diabetes. Many people with MASLD who are overweight but not diabetic are now getting these drugs - especially if they’ve tried diet and exercise without success.
What foods should you avoid with MASLD?
Avoid added sugars, especially high-fructose corn syrup - found in soda, candy, baked goods, and even "healthy" granola bars. Limit processed carbs like white bread, pasta, and rice. Alcohol isn’t a direct cause of MASLD, but it worsens liver damage. Focus on vegetables, lean protein, whole grains, nuts, olive oil, and legumes. A Mediterranean-style diet is the most proven approach.



Just read this after my last bloodwork came back with elevated liver enzymes. I was scared, but this broke it down so clearly. I’ve been trying to cut out soda and processed snacks, and honestly? I didn’t realize how much fructose was hiding in everything. Starting a Mediterranean diet this week - no more granola bars for me.
Wow, another ‘lose weight and you’ll be fine’ lecture. Newsflash: I’ve lost 40 pounds before. Got my liver numbers down for six months. Then life happened - stress, sleep loss, work travel - and it all came back. This isn’t about willpower. It’s about a broken system that’s been exploited by Big Pharma and Big Food. You think a $1,350 shot is the answer? Try living on minimum wage and seeing how ‘simple’ this is.
For anyone considering GLP-1s, don’t skip the dietitian. I’m on semaglutide and lost 18% of my body weight, but what really made the difference was tracking my fructose intake. I used Cronometer for a month - turned out I was getting 40g/day from ‘healthy’ fruit smoothies and flavored yogurt. Cut that to under 20g, and my FibroScan improved faster than expected. Also, walking after meals helps with insulin spikes. Small things, big impact.
I hate how this whole thing gets framed like it’s a personal failure. My liver fat went up after my mom died. I didn’t eat more - I just stopped caring. No one talks about grief, trauma, or depression in these articles. You just say ‘lose weight’ like it’s a switch. But when you’re numb, even cooking a vegetable feels impossible. So yeah, I’m on a drug. And I’m not ashamed.
Excellent breakdown of MASLD pathophysiology. I would like to add that in South Asian populations, visceral adiposity and insulin resistance manifest at lower BMIs than in Western populations. A BMI of 23–25 may already indicate significant metabolic dysfunction. The 7–10% weight loss target should be adjusted accordingly. Also, physical activity should include resistance training - not just cardio - to preserve lean mass during weight loss. The evidence from Indian cohort studies supports this.
THEY DON’T WANT YOU TO KNOW THIS - BUT THE PHARMA COMPANIES ARE MAKING BILLIONS OFF THIS. THEY REBRANDED NAFLD TO MASLD SO THEY COULD SELL DRUGS. 76% OF PEOPLE ON SEMAGLUTIDE GET NAUSEA?! AND YOU CALL THAT A ‘BREAKTHROUGH’?! I’VE BEEN ON IT FOR 4 MONTHS. I’M TIRED. I’M DEPRESSED. I’M STILL HUNGRY. I’M STILL FAT. AND NOW I’M $1,350 IN THE RED. THIS IS A SCAM. THEY’RE PROFITING OFF OUR PAIN.
While I appreciate the clinical precision of this article, I must respectfully note that the framing of MASLD as a purely metabolic condition overlooks the profound sociocultural determinants of health. In many communities, access to fresh produce, safe spaces for physical activity, and affordable healthcare remains structurally inequitable. The recommendation to ‘consult a dietitian’ assumes a level of privilege not universally accessible. We must advocate for systemic change, not merely individual compliance.
STOP WITH THE ‘LOST 10%’ BS!! I’M A VETERAN. I’VE BEEN TO AFGHANISTAN. I’VE BEEN THROUGH MORE THAN YOU’LL EVER KNOW. I’M NOT SOME ‘OBESITY CASE STUDY’ FOR YOUR PHARMA ADS!! I’M ON SSDI BECAUSE OF PTSD AND CHRONIC PAIN. YOU WANT ME TO WALK 30 MINUTES? TRY WALKING WHEN YOUR KNEES ARE GONE AND YOUR MIND IS BROKEN. THIS ISN’T ABOUT LIVER FAT - IT’S ABOUT A SYSTEM THAT ABANDONS PEOPLE LIKE ME AND THEN TELLS US TO FIX OURSELVES. I’M NOT A PROBLEM TO BE SOLVED - I’M A HUMAN BEING!!
Hey David, I hear you. I’ve been there - chronic pain, meds, depression. I didn’t lose weight until I stopped trying to ‘fix’ myself and started focusing on small, sustainable moves. I started with 5 minutes of stretching every morning. Then added a walk after lunch. Took me 8 months to get to 10% loss. The drug helped, but it didn’t do it alone. And honestly? The side effects sucked at first. But I kept going because I wanted to live longer than my dad. You’re not alone. And you’re not broken. You’re just fighting a system that wasn’t built for you.